C19 is an unprecedent phenomenon because it has fostered an unscientific thinking epidemic in the public fueled by the media. It is truly shocking what is happening in the media – science is being utterly trashed and rehashed to create junk news narratives to control people with fear.
People fear things they don’t understand. Today’s blog is designed for you to understand things better to show you there is nothing to fear if your redox levels are good before you come in contact with C19.
Higher ROS levels are also linked to higher levels of viral infection and replication.
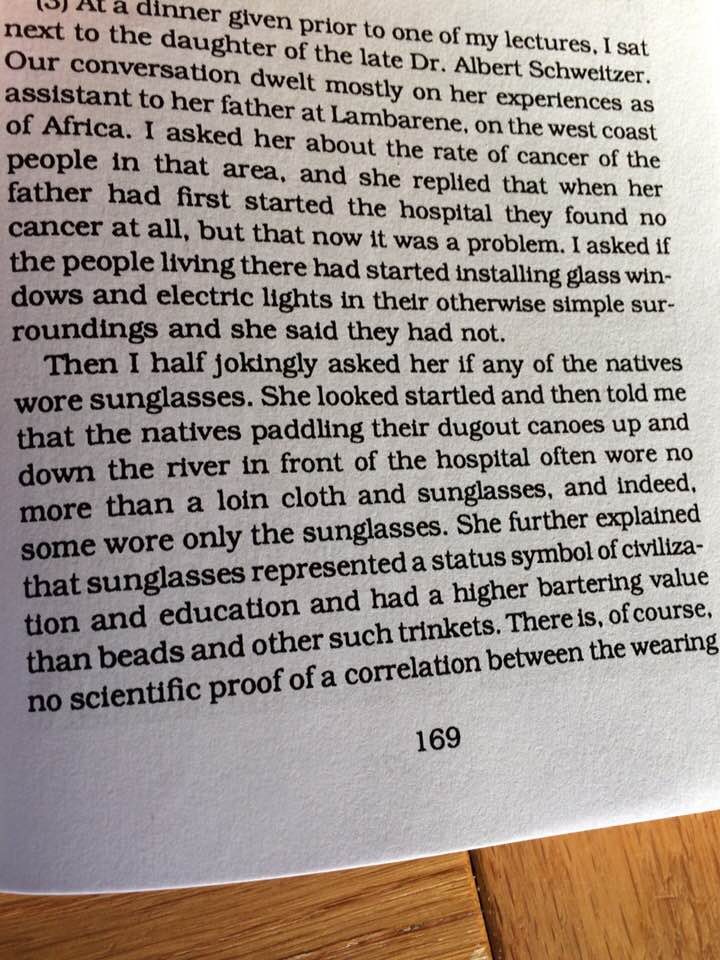
What heme protein in your blood controls ROS levels as a defense? CATALASE.
Researchers have tested the use of stabilized catalase to regulate the level of ROS in virally infected cells. ROS are oxygen metabolites that are potent oxidants, mostly generated by the electron transport chain in the mitochondria and cytochrome P450, but also via oxidase enzymes found in many cells, especially endothelium and phagocytes.
Typically, the process of ROS generation begins with superoxide anions, which being unstable are rapidly converted to H2O2 or hydrogen peroxide, via superoxide dismutase (SOD3). H202 is known to cause feedback regulation of some of the dehydrogenases on the respiratory chain.
H202 may be converted to oxygen and water through the enzyme catalase, or to HOCl via myeloperoxidase (MPO), or to water through glutathione/glutathione peroxidase complex (GSH/GPX).
Whenever antioxidant enzymes are deficient, or if ROS are produced in excessive amounts, H2O2 may accumulate in the tissues, causing oxidative protein damage and producing more ROS. Thus, it is important to get rid of this chemical when it is present in large amounts.
The ROS is part of the body’s weaponry against infections, and also an essential part of the body’s signaling mechanism. Its generation is essential to recruiting leukocytes to wounds, to modulate the immune response. Thus, it is needful to mitigate the excessive production of ROS rather than suppress them altogether. This could also restore immune function to normal.
The antioxidant catalase is the most abundant and effective enzyme to break down H2O2 in our blood plasma. It is commonly found in the liver, red cells, and the alveolar cells of the lung. It is able to decompose 107 molecules of H2O2 within a second. However the problem is that this enzyme is highly unstable to topologic effects.
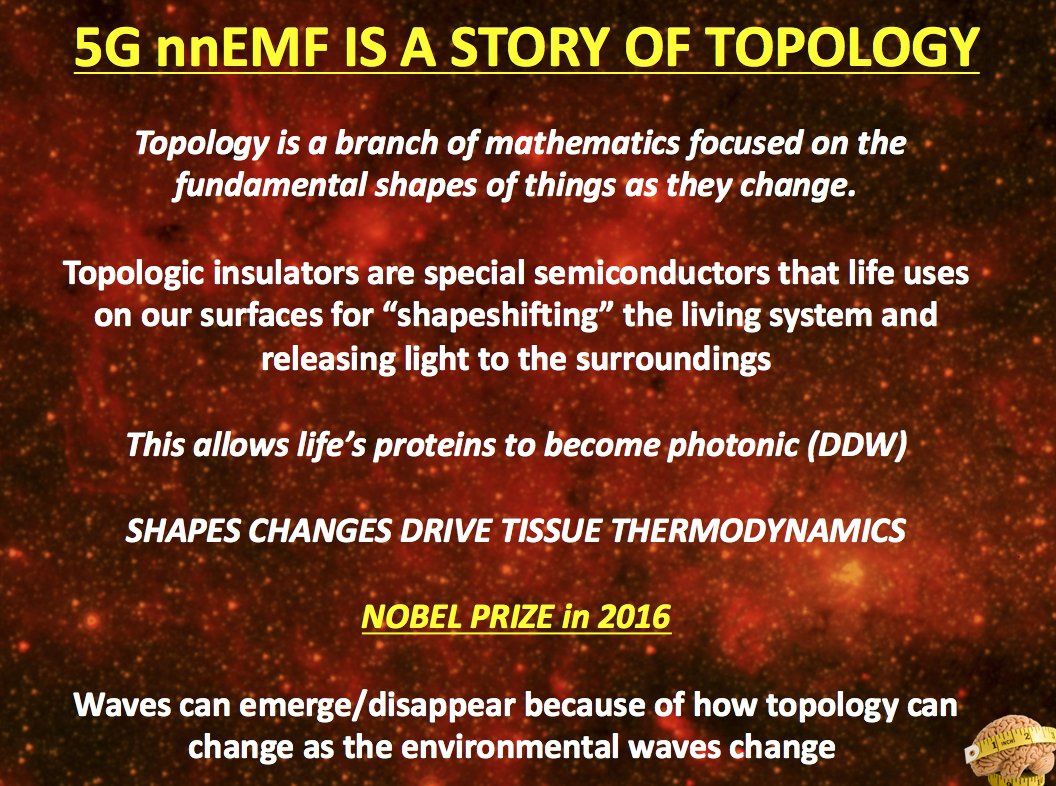
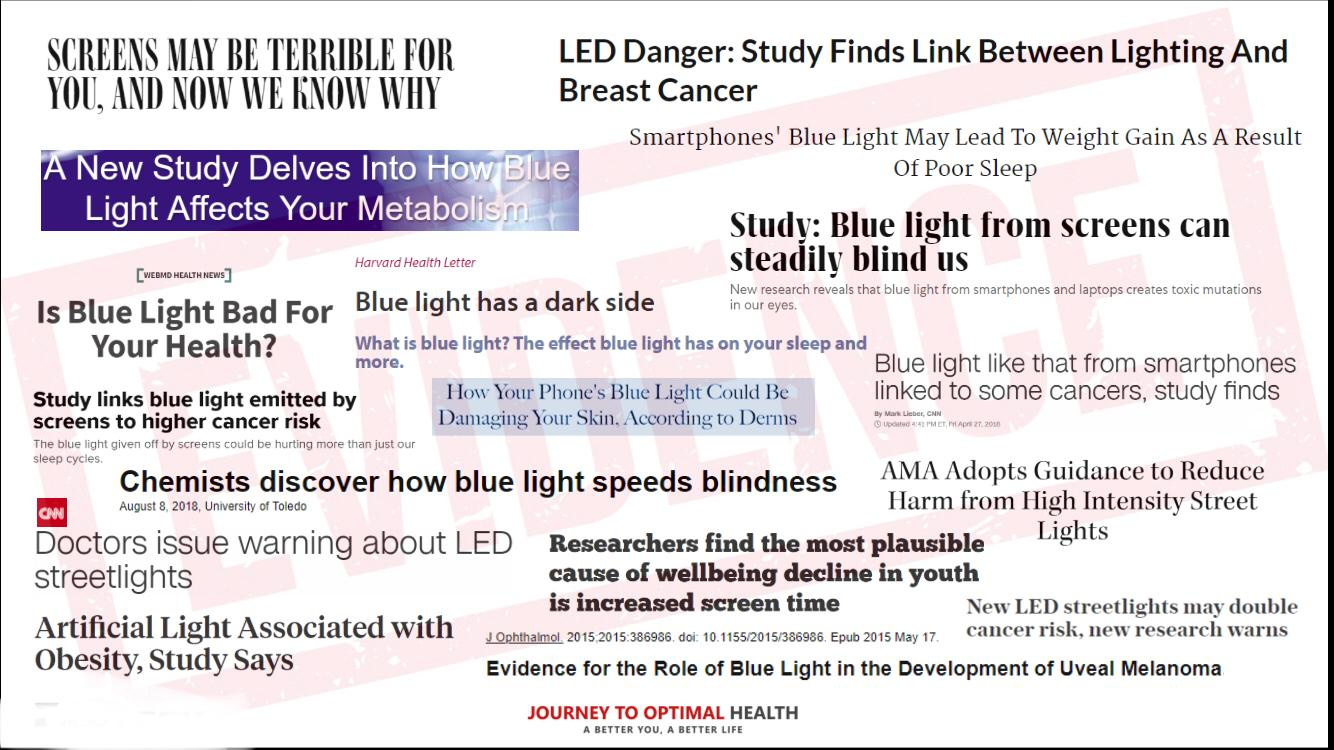
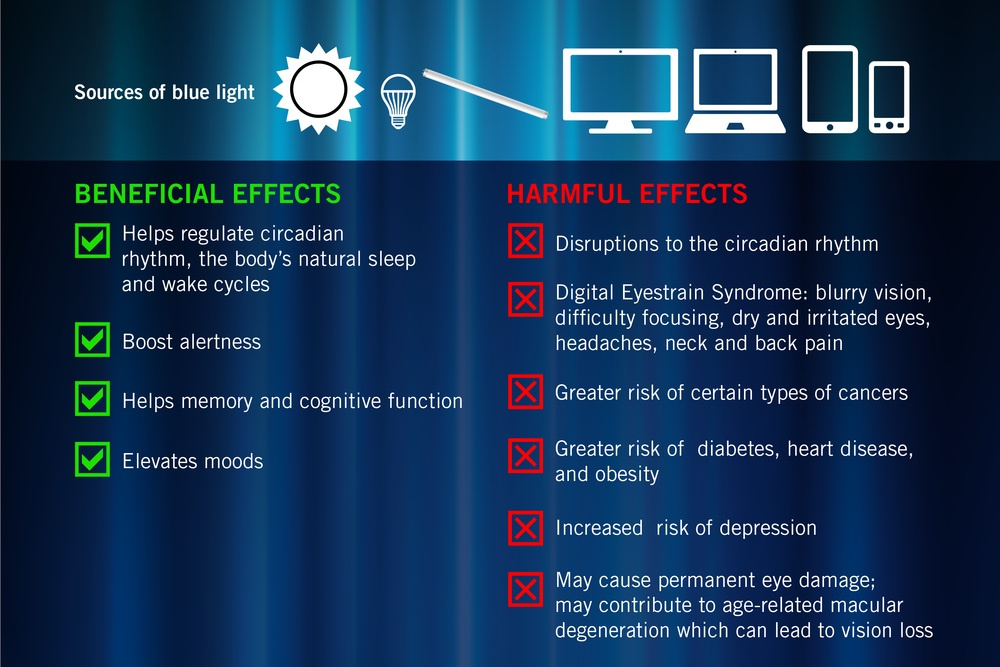
5G is another type of man made light wave that causes problems at surfaces.
When skin is altered topologically can you make Vitamin D normally?
Nope.
Vitamin D is absolutely necessary for people’s lives. Without it, we can’t live. It’s critical to activate T-cells as this hyperlink shows: https://tinyurl.com/gsrc53x
The Sun allows us to create vitamin D via our skin surface and is thus the best vaccine against C19.
Anyone who is injured by c19 has betrayed or a naive immune system. This may be viral, bacterial, fungal/mycotoxin, irritated bowel, urinary tract disease, metabolic disease, MS, leprous, malnutrition, sepsis, celiac disease, urinary tract infection, and or frequent infections.
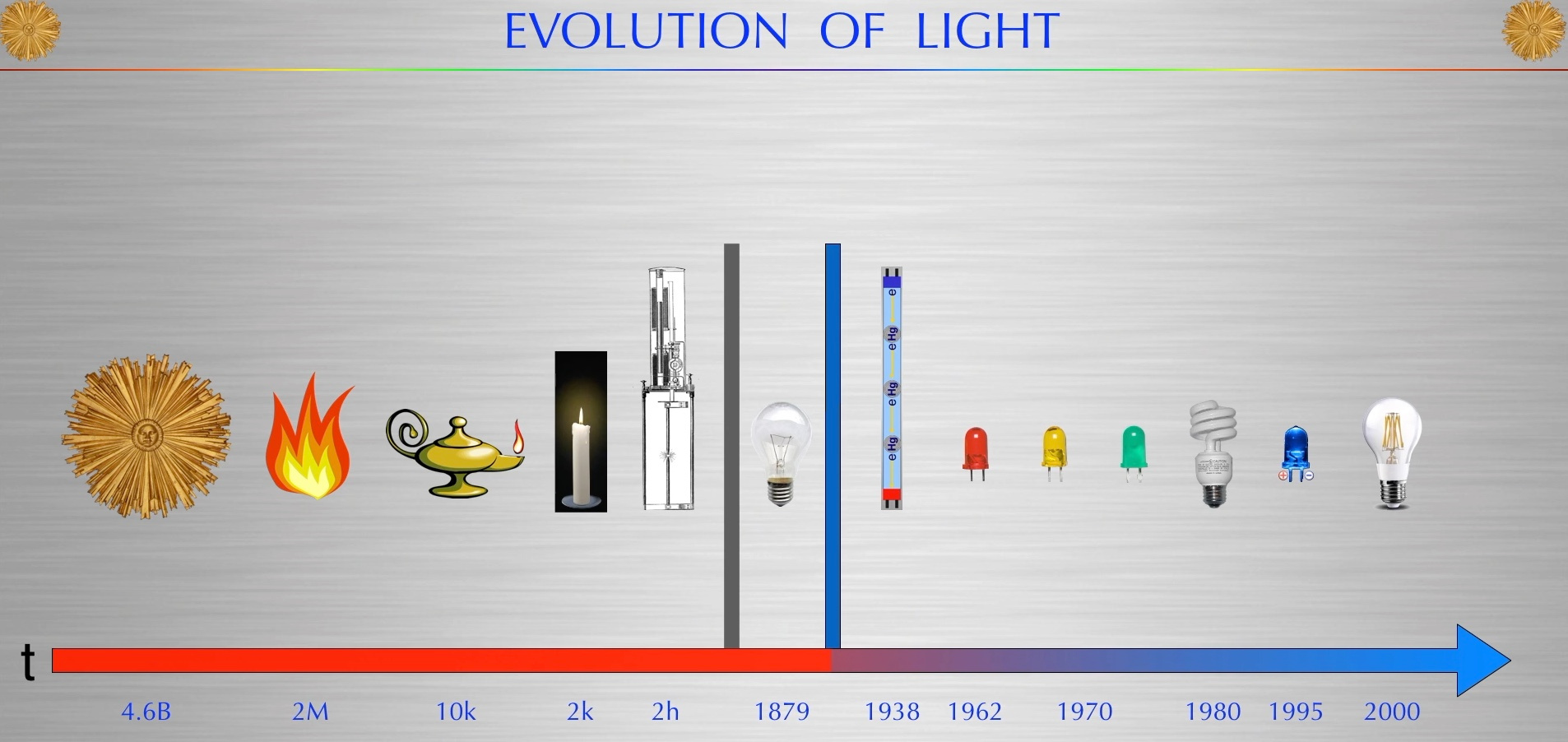
Light breaks a lot of human assumptions in science.
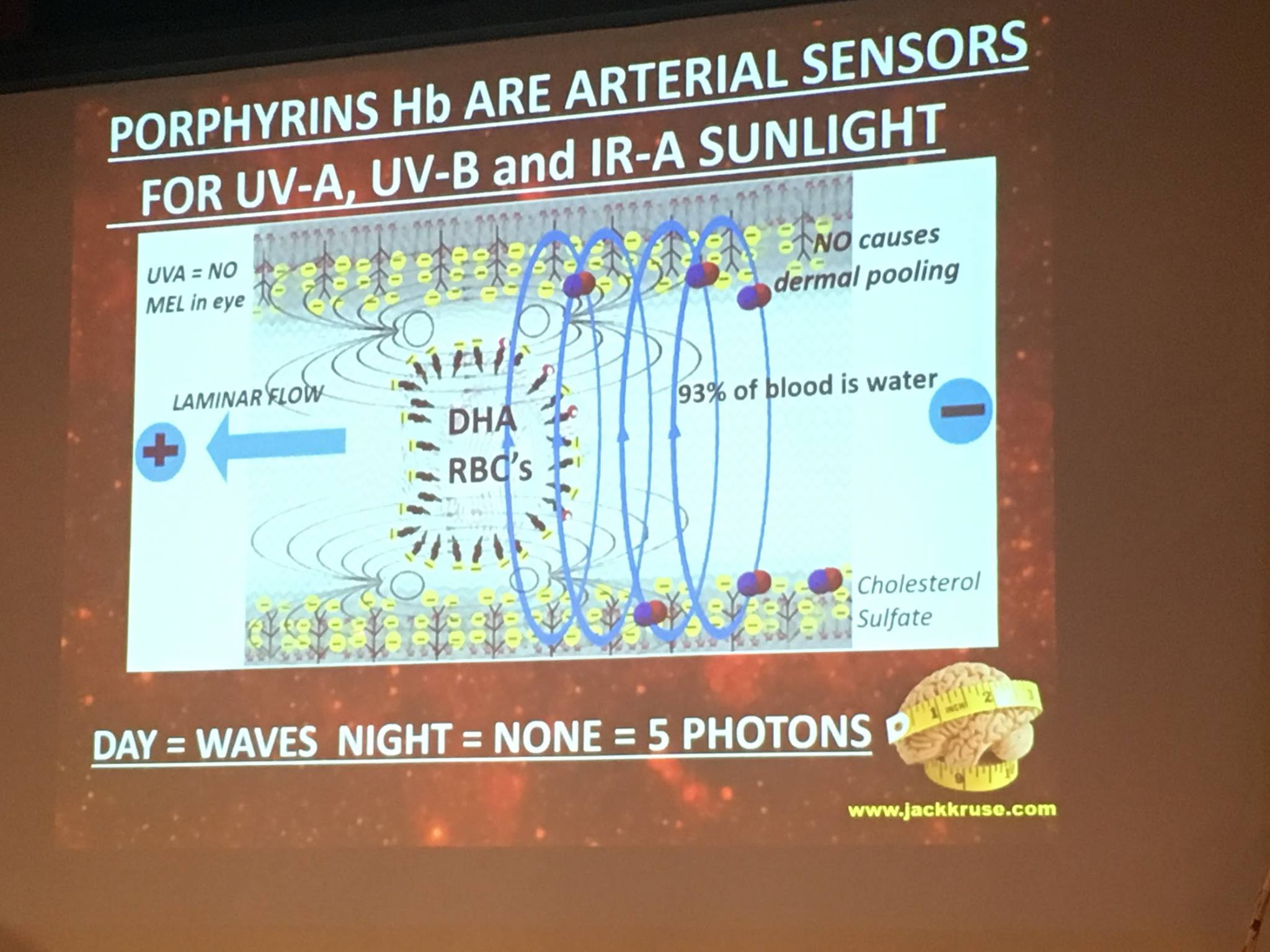
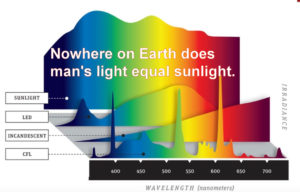
Full-spectrum terrestrial with UVA and UVB de-magnetizes (or de-gausses) the blood plasma which has a myriad of collateral effects. It improves T cell function in the adaptive immune response to limit cytotoxic storms so common in C19 cases in those with low Vitamin D levels in ICUs.
Did you know sunlight alters catalase levels seasonally which affects the free radical H2O2 in your blood plasma to work optimally?
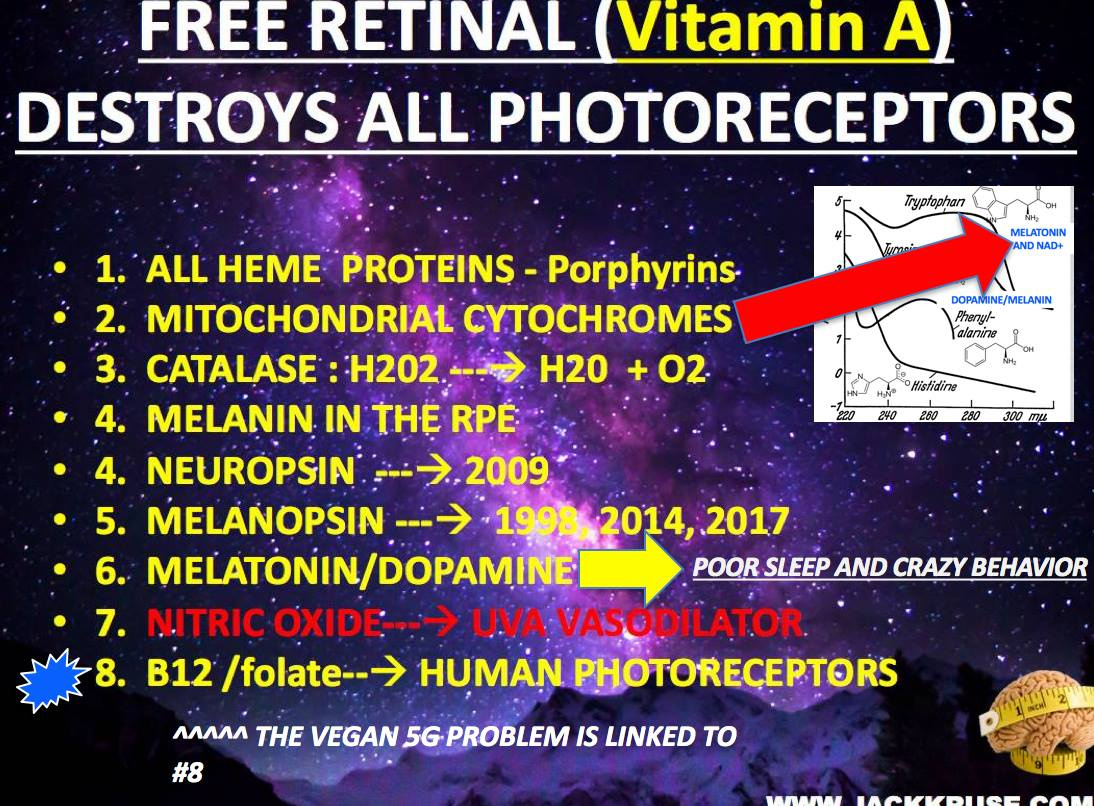
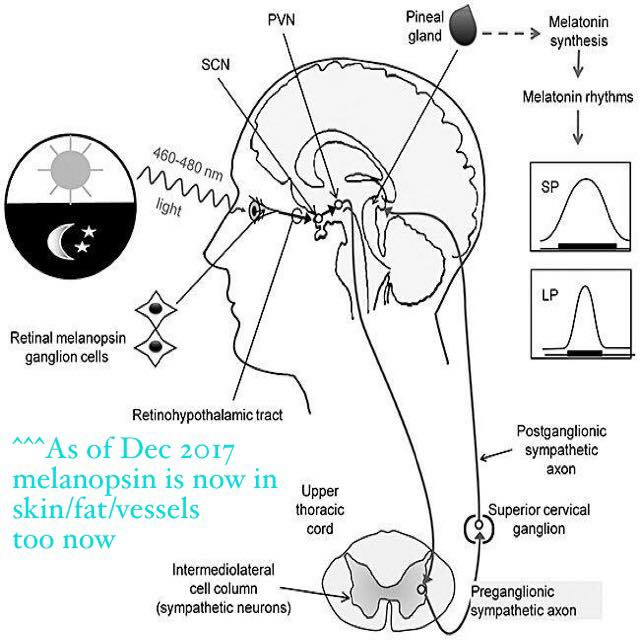
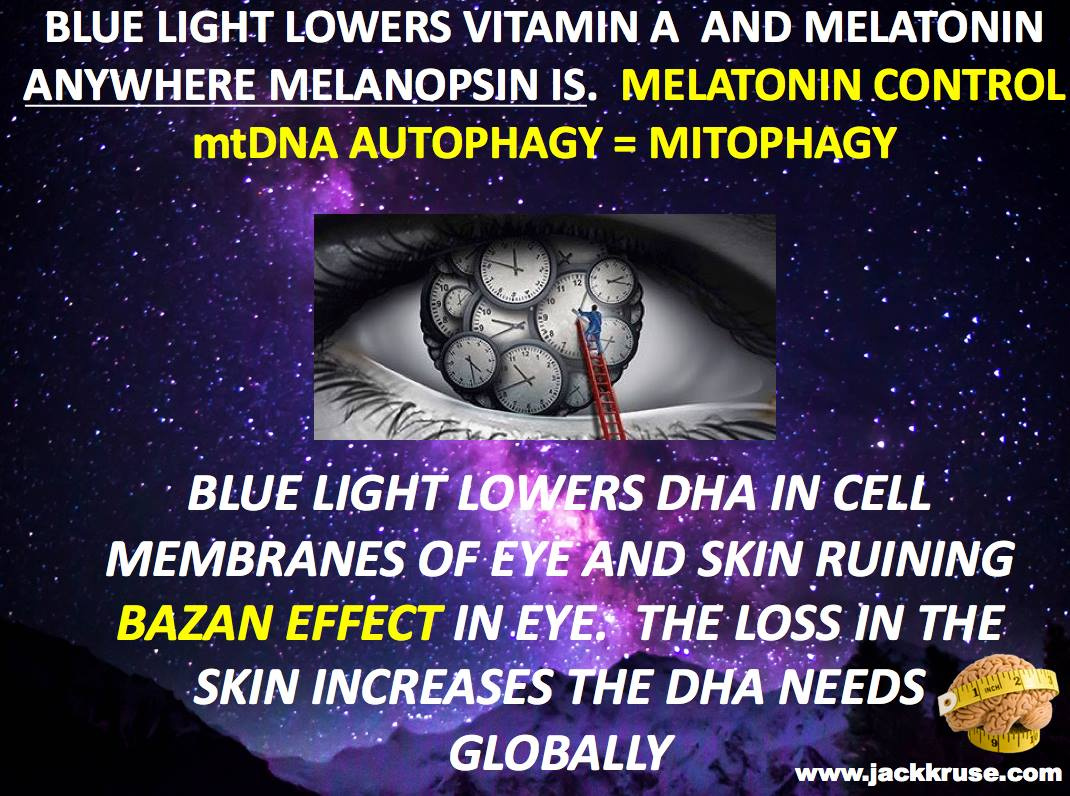
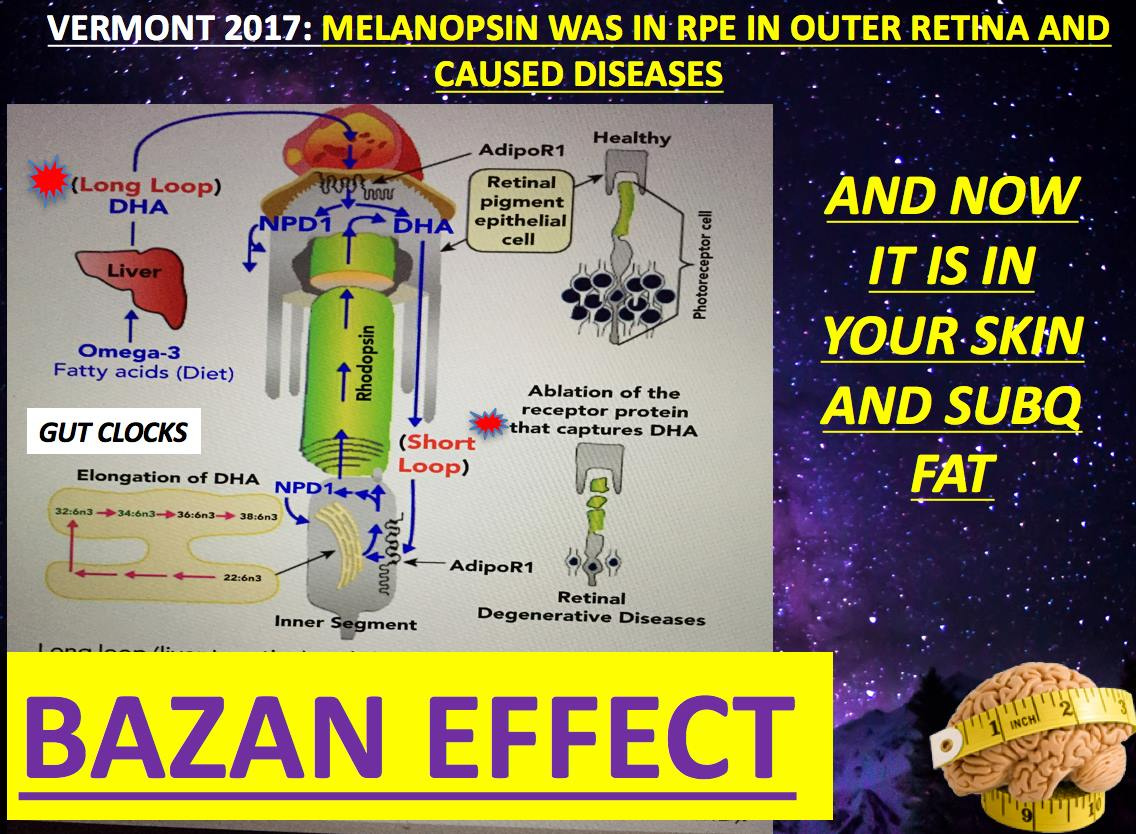
CATALASE: is a heme containing enzyme that mitochondria use to control oxygen using water as its medium. Recall all heme proteins are destroyed by melanopsin damage and C19.
Heme containing enzymes (catalase and peroxidase):
Catalase catalyzes the decomposition of hydrogen peroxide to give water and oxygen.
2H2O2 → 2H2O + O2
Peroxidase (POD): Peroxidase catalyzes the dehydrogenation of a large number of organic compounds such as phenols, aromatic amines, hydroquinones.
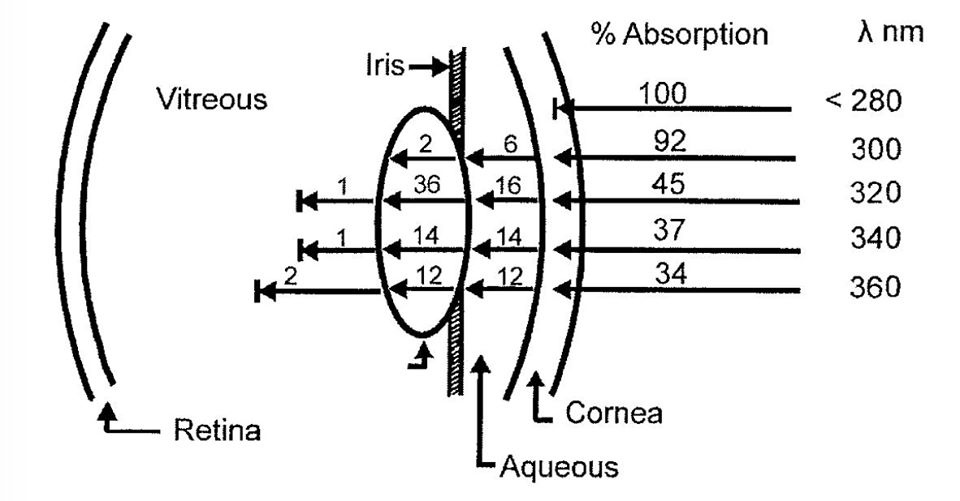
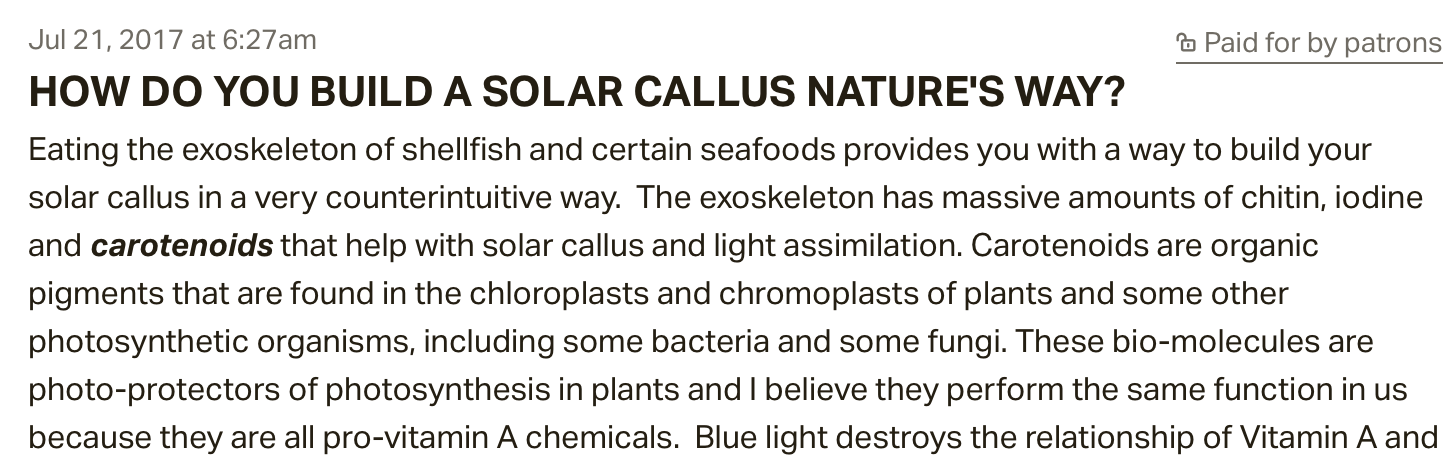
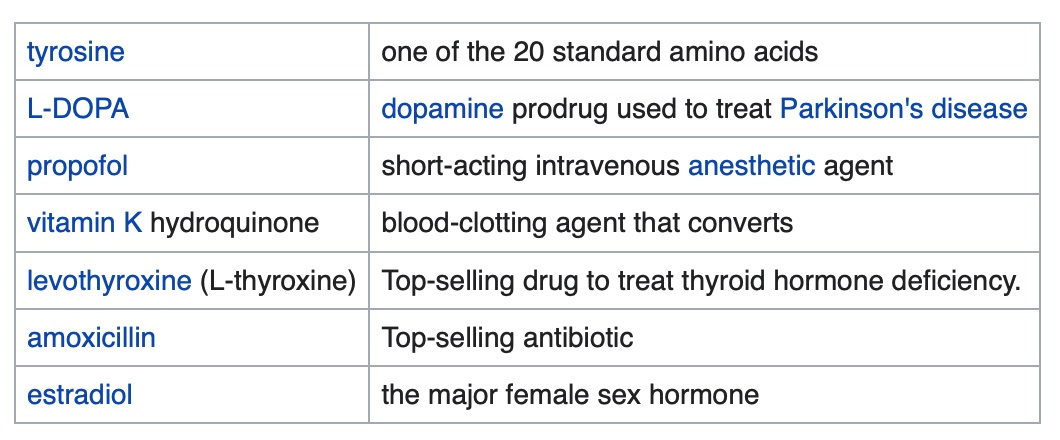
C19 sepsis creates phenols. Short-term exposure to high levels of phenol is known to cause irritation of the respiratory tract. Phenols are oxidized by peroxides to hydroquinones. Hydroquinone cause a lose of melanin in the skin. Melanin is made from tyrosine which is a phenol in humans. This disables absorption of UV light and is common in vitiligo and people who do not have a solar callus from proper sun exposure.
WHAT ARE SOME PHENOLS YOU MIGHT HAVE HEARD OF?
Yes, hypoxia from a LACK of sunlight destroys these chemicals in your body. Do you still think avoiding the sun is wise arm with this new knowledge?
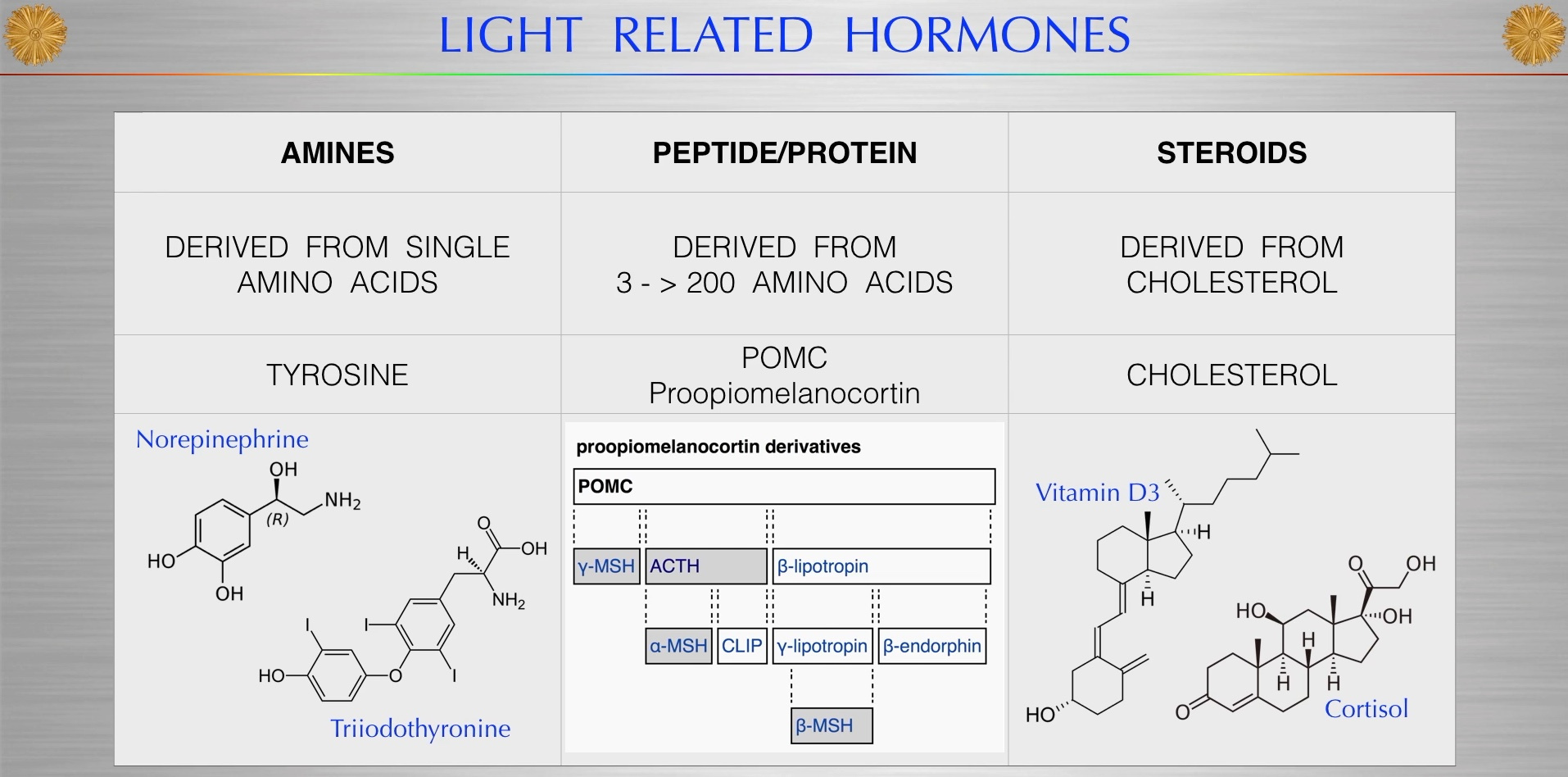
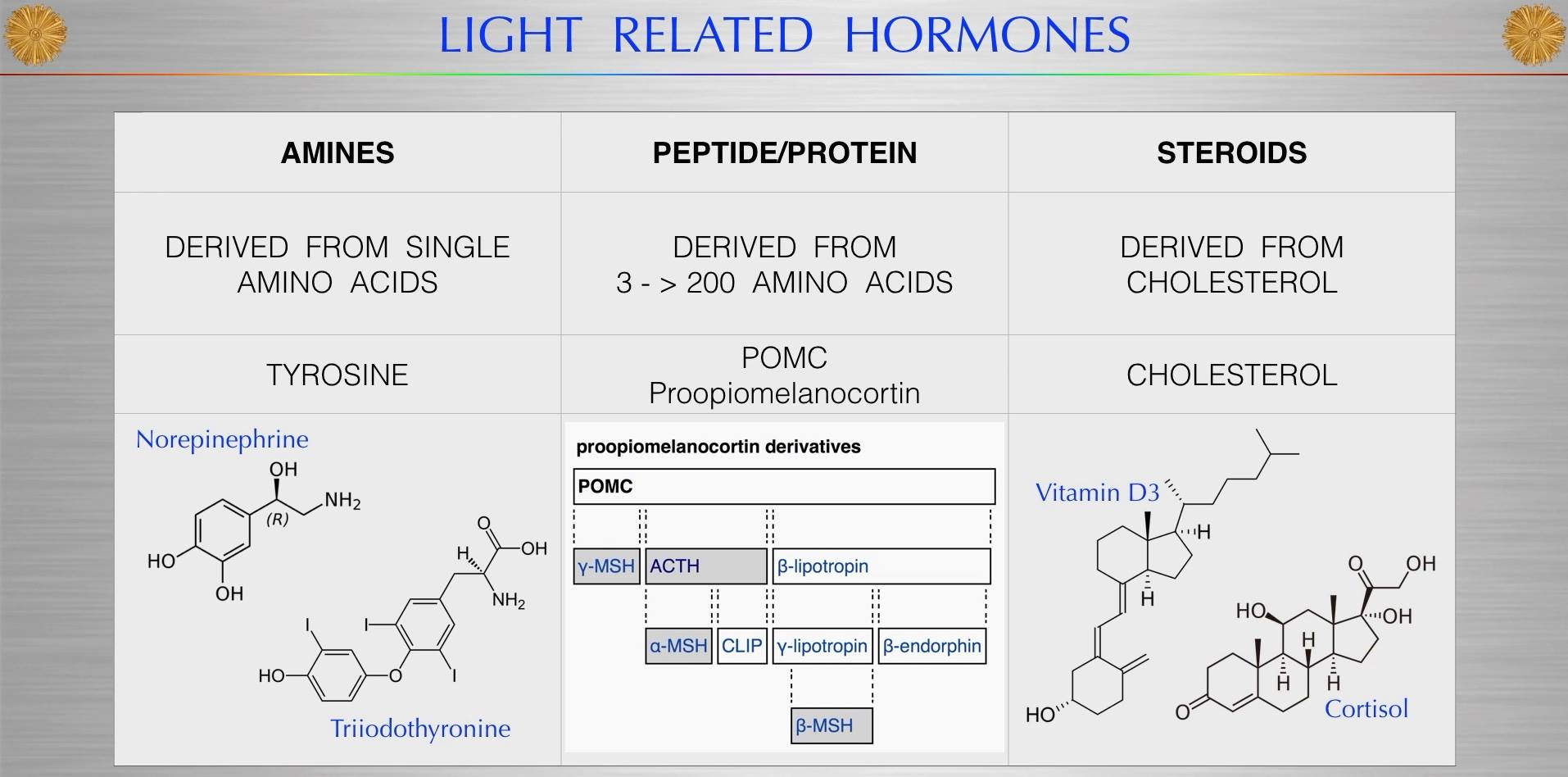
Biogenic amines are also destroyed by a lack of sunlight induced hypoxia. A biogenic substance with one or more amine groups.
Some prominent examples of biogenic monoamines include:
- Imidazoleamines
- Histamine – a substance derived from the amino acid histidine that acts as a neurotransmitter mediating arousal and attention, as well as a pro-inflammatory signal released from mast cells in response to allergic reactions or tissue damage. Histamine is also an important stimulant of HCl secretion by the stomach through histamine H2 receptors. UV lowers histamine in cells.
- Indolamines
- Serotonin – a central nervous system neurotransmitter derived from the amino acid tryptophan involved in regulating mood, sleep, appetite, and sexuality.
- The three catecholamine neurotransmitters:
- Norepinephrine (noradrenaline) – a neurotransmitter involved in sleep and wakefulness, attention, and feeding behavior, as well as a stress hormone released by the adrenal glands that regulates the sympathetic nervous system.
- Epinephrine (adrenaline) – an adrenal stress hormone, as well as a neurotransmitter present at lower levels in the brain.
- Dopamine – a neurotransmitter involved in motivation, reward, addiction, behavioral reinforcement, and coordination of bodily movement.
Trace amines (endogenous amines that activate the human TAAR1 receptor)
- Phenethylamines (related to catecholamines):
- Thyronamine compounds:
- Tryptamine
Other biogenic monoamines
- Trimethylamine
- Trimethylamine N-oxide
- Indoleamines
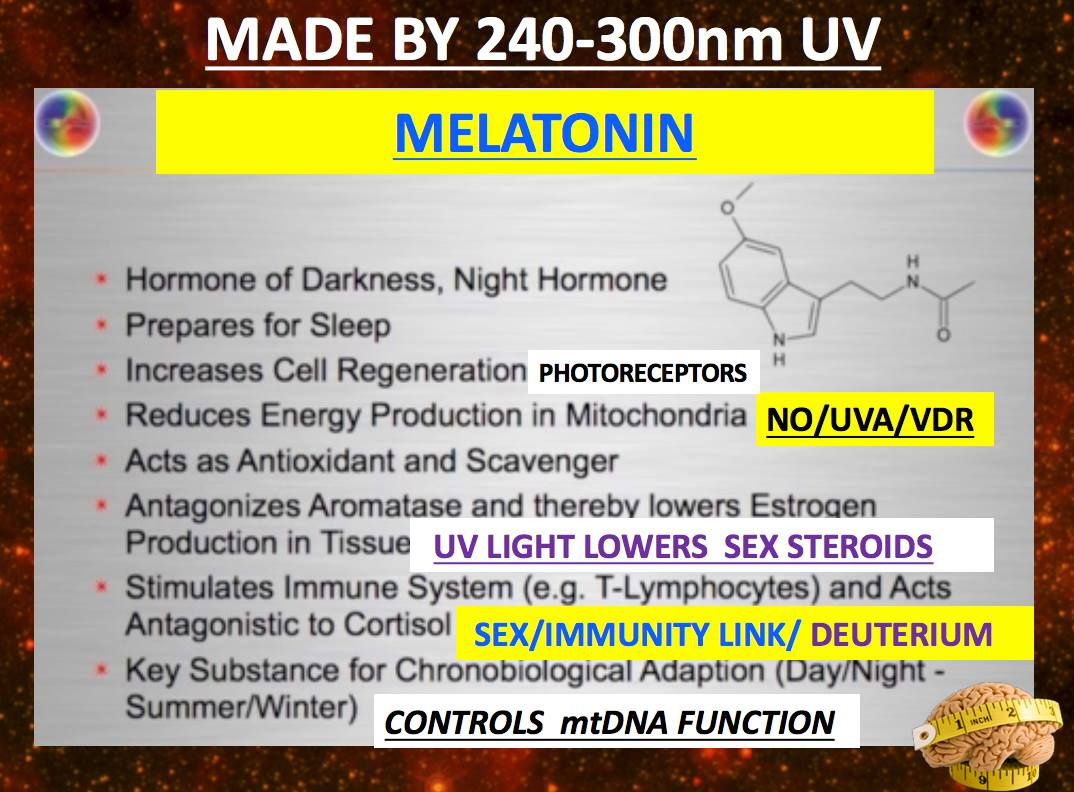
- Melatonin : BIGGIE HERE FOLKS!
- 6-Hydroxymelatonin
- N-Acetylserotonin
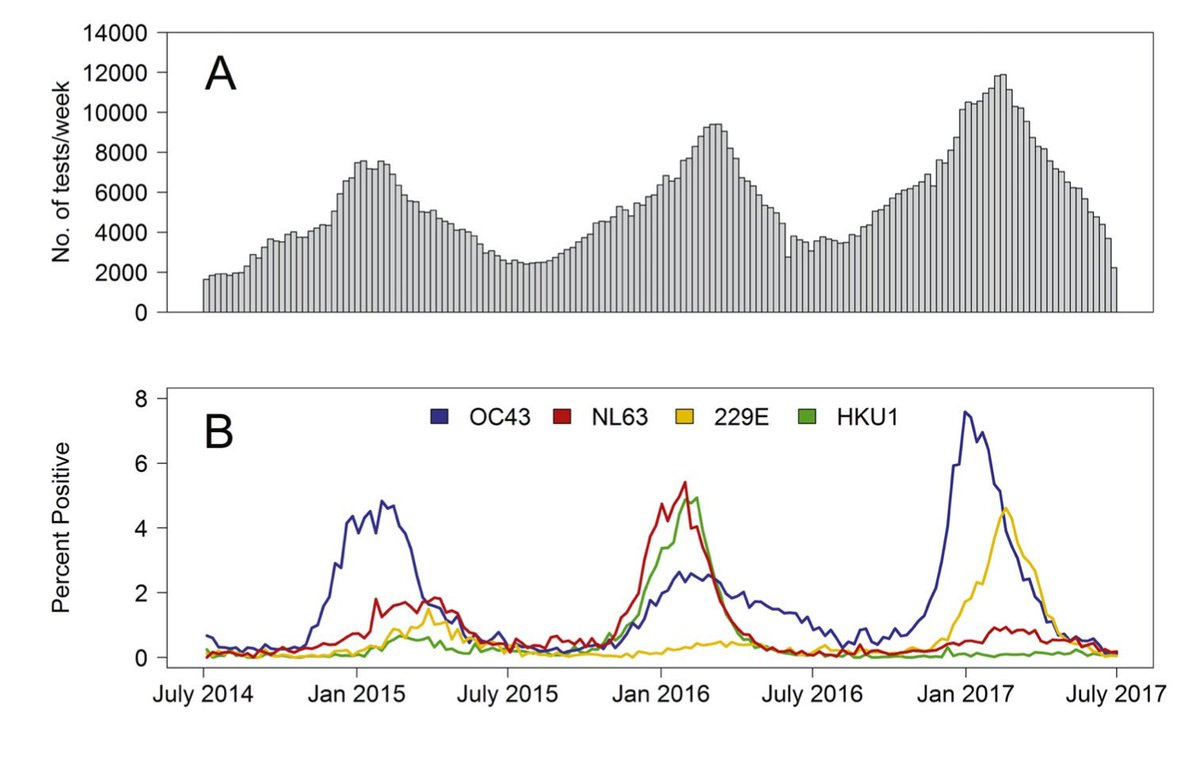
- Sun exposure resulted in a seasonal variation of the catalase activity in stratum corneum, with low activities in summer and higher activities in winter for the same person, whereas superoxide dismutase activity in stratum corneum did not seem to vary in those conditions. Exposure of human skin to broadband ultraviolet-A resulted in a dose-dependent deactivation of the catalase activity in stratum corneum within 24 h, whereas exposure to ultraviolet-B had no effect.
Why is this important? WHEN catalase is added to hydrogen peroxide, there is an initial rapid evolution of oxygen and this affects local mitochondrial function. This effect lasts for about two minutes, depending on the peroxide free radical concentration. After this, oxygen is given off at a steady rate which slowly decreases in the course of an hour. This is one way UV light increases venous oxygen tensions in humans. We actually can breath through our skins. This can help hypoxia of disease as we see in C19. It turns out natural sunlight exposure also keeps our blood chemistry around a pH of 7. This creates the most oxygen from the interaction of catalase and H2O2. I often use exogenous hydrogen peroxide directly on the brain when I feel hypoxia is a problem for the brain. I also know that the use of hydrogen peroxide on the neocortex has the chance to stimulate the production of melatonin in the hypoxic brain to lead to quicker recoveries as I laid above. Often this occurs during trauma surgery or brain tumor surgery.
Yes, hypoxia just from a LACK of sunlight destroys these chemicals in your body made from tyrosine like melanin, thyroid hormones, estradiol, norepinephrine, Vitamin K2, and dopamine. Do you still think avoiding the sun is wise now that you know better?
WHY DO C19 patients struggle to heal wounds and clot blood?
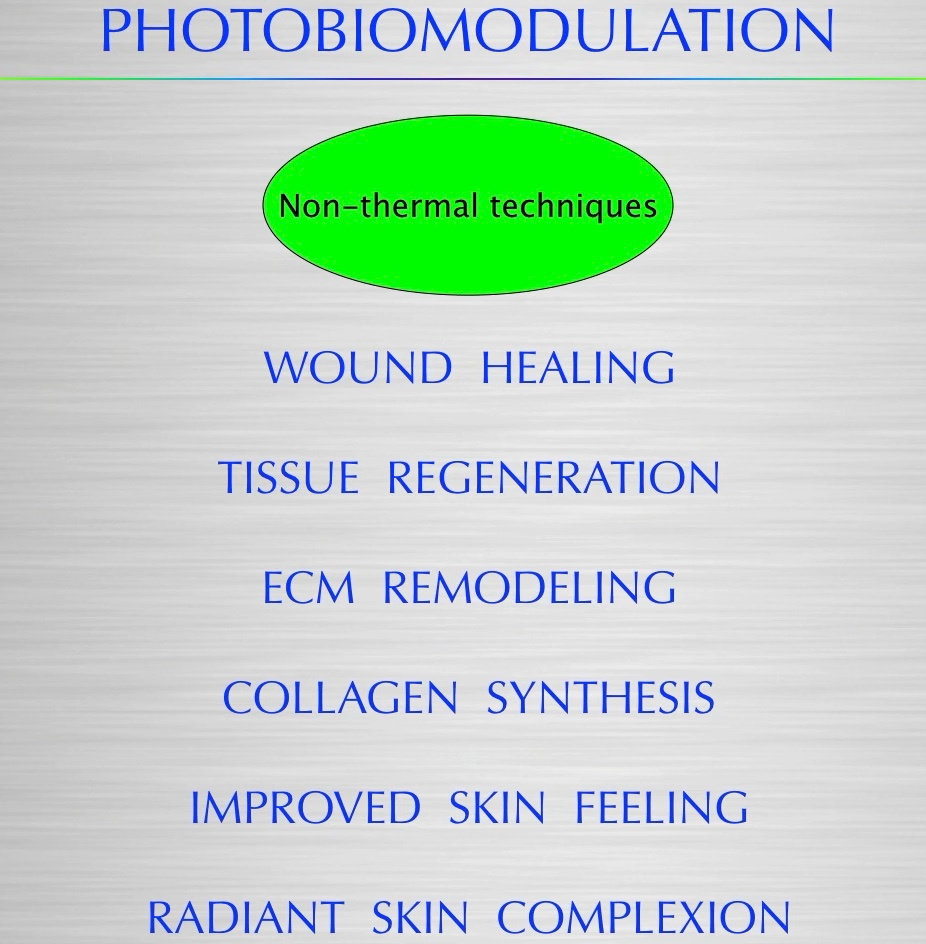
The key is understanding the lack of wound healing in C19 is knowing that the switch that controls healing and regeneration is 100% electromagnetic because of light. A lack of sunlight causes a lack of healing.
During day the DC current flows negative to positive in tissues. Light via your eye, causes the pineal to release serotonin. During night time a lack of light via your eye causes you pineal to release melatonin. This is an electrical phenomena done by the electric and magnetic portions of light in their waves. Your CNS is most negative tissue in your body. During night time the current reverses direction and the DC current disappears. This is likely due to the affect of adensine and magnesium changes in the matrix of mitochondria to help us regeenrate. Most people have no idea the switch is electromagnetic (presence or absence of light does it) that controls a macrophage protein that acts in the MAM of the mitochondria and the ER of the Golgi. It is called MCP-1. In tissue damage, the first signal is a loss of the DC electric current and activation of cGMP and this stimulates the INFLAMMATORY cascade to clear damage. After a period of time determined by the electromagnetic signal, the same electromagnetic signal then uses a different second messenger to stop the inflammatory chemokine reaction and begin repair using cAMP. The regeneration begins when the DC electric current in the tissue is restored and then mitophagy and autophagy drive the healing. This is all increased by sunlight and cooling. One of the best free health tips I can give ANYONE who wants to live a healthy and long life:
learn these 2 words – Autophagy and Apoptosis. Melatonin levels control these two change programs in cells. Given what you learned above, you might be seeing why this is critical now.
Learn what they mean, and then learn how you can manipulate your body to optimize these 2 crucial cellular functions through lifestyle. Then do it!
Think of your cells as a bunch of shiny Lamborghini cars. Built for optimal function.
Sometimes, your carburetor or your battery dies in your Lamborghini. When that happens, you certainly aren’t going to throw it out, are you? You just fix what is broken and replace the parts of the car that are not functioning well. And voila. Like brand new.
That’s AUTOPHAGY.
But sometimes the damage to your Lamborghini is beyond repair. The engine is ceased and unrepairable. The body is a disaster. The transmission is on its last leg. I this case it might be better just to trash it completely and get a new car by replacing it.
That’s APOPTOSIS.
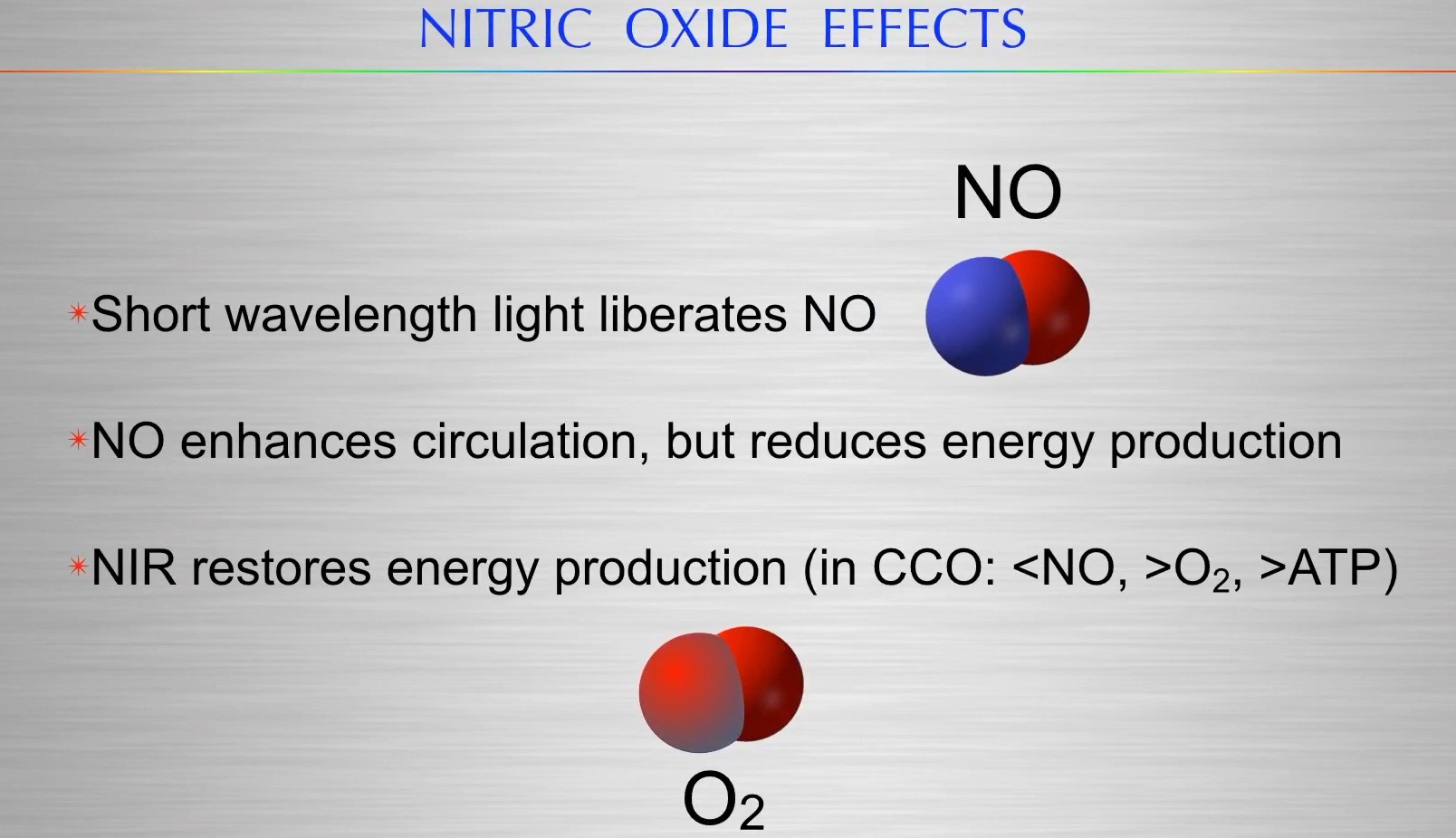
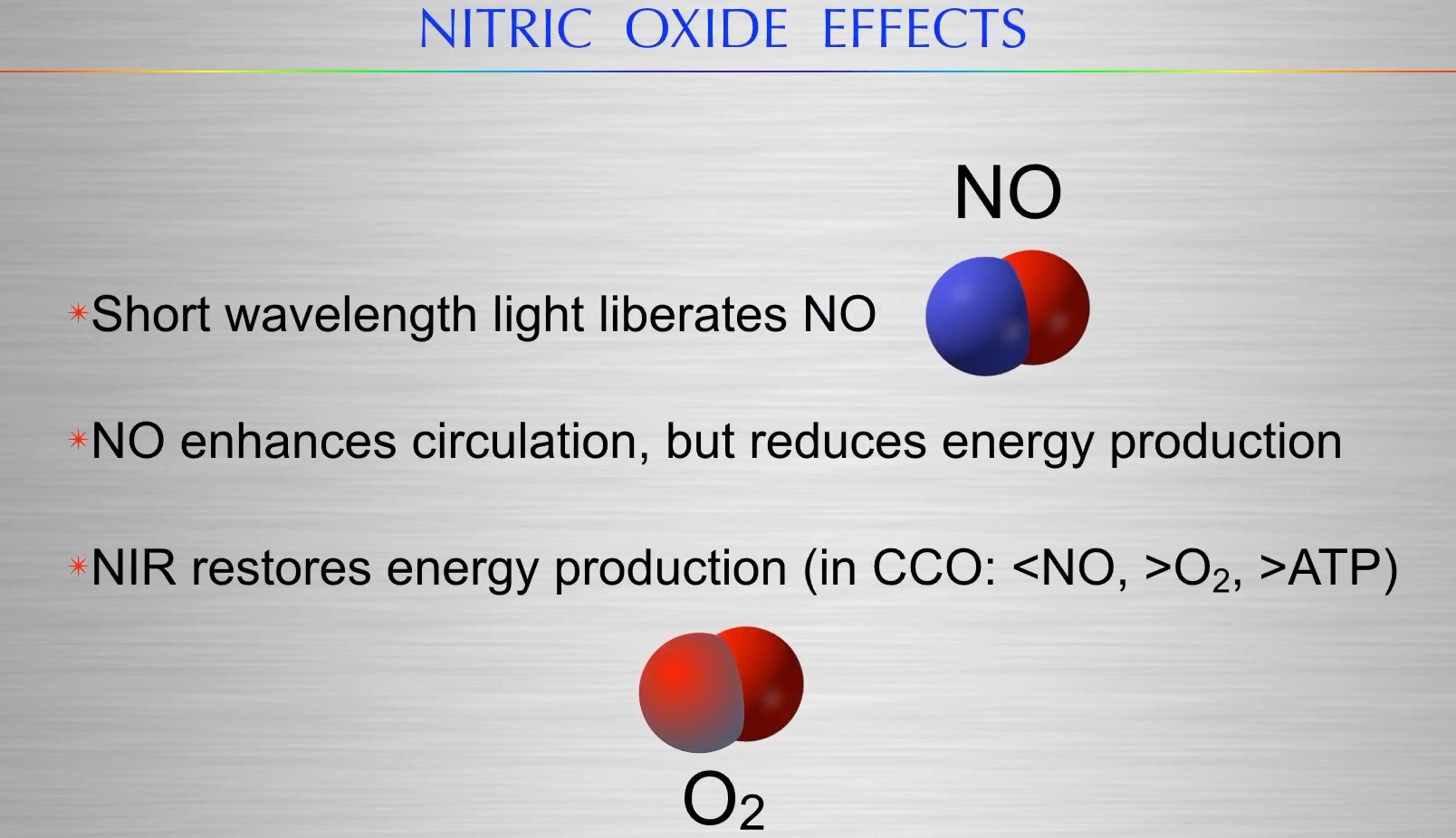
If autophagy and apoptosis are working well in your body, you will have optimally functioning cells, organs, and energy levels. The electromagnetic signals in the ECT control this process especially at CCO = cytochrome 4. Restoration of metabolism occurs when regeneration of the damaged tissue mitochondria begins repairs using information in light called orbital angular momentum (OAM) to repair deficits and tumors can respond without drugs to sunlight because of how sunlight acts on kinases and Cytochrome C oxidase (red light) with nitric oxide (NO) from UVA light. (see Cite below)
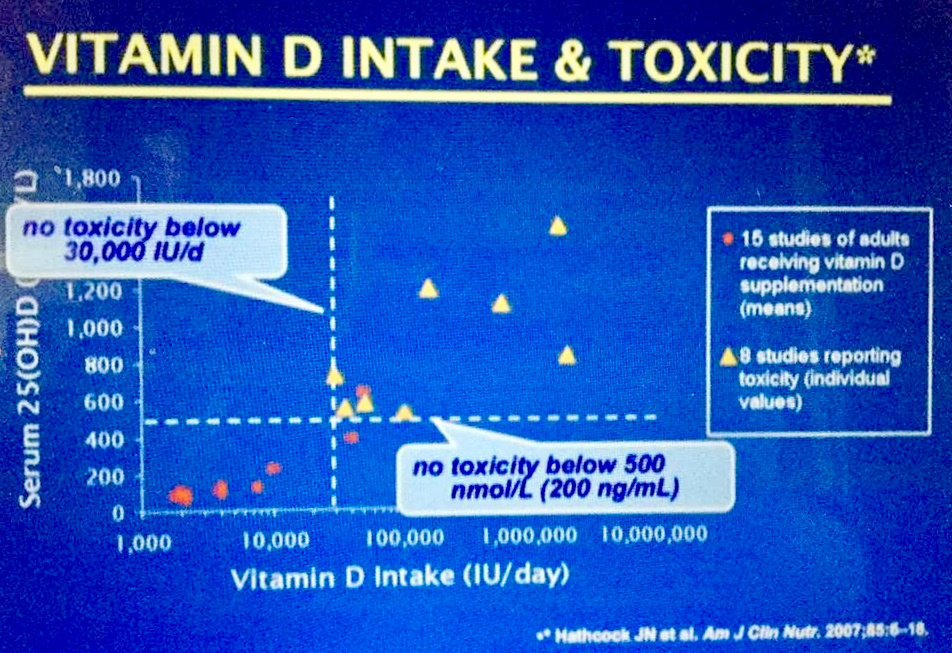
SCIENCE GEEKS: Energy and information in the living state are normally coupled and quantized by light and oxygen levels. Once apoptosis control is lost, we also lose control of beta oxidation and protein metabolism is lost. This is how adding exogenous substrates (blue light for solar light) can ruin a coupled feedback loop to lead to disease. a lowered Vitamin D level is a clue to the ICU doc that this has occurred and you better take it into account.
In E = mc^2, Energy represents information and energy and we know this from physics and information theory. Both energy and information are transferred in quanta. They are not continuous.
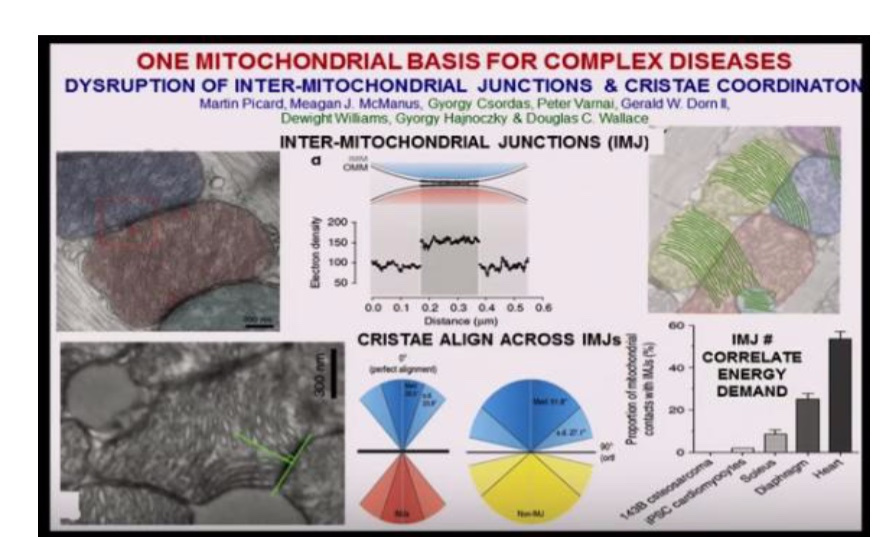
The hydrogen isotope isoforms (deuterium) inside the matrix and cytosol are affected by the physiology of fumerase. This is impacted by red light exposure on the hydration cell of magnesium ions in the matrix that is gel like because of the effect of magnesium on the viscosity of the environment. The more Mg2+ the more gel like the matrix is and the better energy is made by the cristae which all line up perfectly as this picture shows. Magnesium in the matrix hydrates it to form a gel which controls the size and shape and arrangement of the cristae to allow it to oscillate at 100Hz. That is optimal beta oxidation as Meagan McManus showed.
The matrix isoforms stops the TCA cycle from performing its cycle because of the kinetic isotope effect of deuterium. In the cytosol, the urea cycle also uses fumaerase to add water in amino acid metabolism. This is why protein metabolism is a problem in some cancers. It is also why fat burning can be issue as well. If water recycling is broken in the TCA cycle and urea cycle, because of a defect in fumarate hydratase you only can use glucose to build substrates. When fumarate hydratase is defective fumarate rises and AMPK is activated to increase glucose metabolism to keep ECT functioning for cancer cell’s energy flux.
Restoration of metabolism repairs information deficits and tumors respond without drugs. High dose IV Vitamin C with a quinone (Vitamin E or K) can remove deuterium to improve hydrogen flows to stimulate apoptosis and re-establish the ability of T cells to get rid of cancer cells or viral cells. This process is linked to the function of cytochrome c oxidase under the power of the infrared part of the spectrum of terrestrial sunlight by controlling the unfolding of histidine residues of cardiolipin. Red light moves things with mass, and it alters the protons in the hydrogen bonds to stimulate the energy of activation of performing this task at the speed of light with little need of ATP. Information quanta in the light affects the proton conduction to control this gating mechanism in cytochrome C oxidase.
The same thing is true or methylene blue and Szent Gyorgi wrote a paper about this in 1936 in Nature. Hypoxia-inducible factor (HIF) is stabilized in fumarase-defective cells, but protection from apoptosis is a HIF-independent mechanism. Activated kinases regulate cell survival at different levels. Few realize sunlight activates kinases. It turns out the members of the Bcl-2 family are affected by fumerate hydratase suppression by deuteration. Pro- and antiapoptotic activities of Bcl-2 family members are regulated at either the transcriptional or posttranscriptional level by the information quanta in electrons and protons.
MATRIX DEUTERIUM CONCENTRATION AND THE ENDO-cannibinoids IS A SOLAR DRIVEN MECHANISM
Proteins released from the mitochondria actually trigger apoptosis and the decision to commit suicide has now been traced directly back to the mitochondria. The ECS are another lipo-protein molecule system that are important in controlling apoptosis. Cannabinoids are a class of chemical that is well known to inhibit mitochondrial respiration.
The ECS system is also stimulated by early AM sunlight to improve mitochondrial function via apoptosis.
Cellular disorganization always manifests in hypoxic diseases like C-19 before death; illness comes before death in most living sequences unless we are talking acute trauma. This points out why the information side of the tissue organization via the free radical signalling is as important as energy flux in a cell to maintain wellness. When hypoxia manifests is amplifies the COX-2 enzyme in cells. This amplification is due to the liberation of many deuterium atoms from the polyunsaturated lipids in the mitochondrial membranes. Deuterium bring energy production in the matrix to a screeching halt because of its kinetic isotope effect on all TCA intermediates. Solar exposure stabilizes cell membranes.
Research has shown us that the type-1 cannabinoid receptor (CB1) is present at the membranes of mitochondria (mtCB1), because it directly controls cellular respiration and energy production. How does it do this? It controls the flow of deuterium from the PUFA’s used to build the two membranes inside of mitochondria. Through activation of mtCB1 receptors, endogenous endocannabinoids decrease cyclic AMP concentration which is the base substrate needed for ATP production. It also lowers protein kinase A activity, complex I enzymatic activity (NAD+) and respiration in neuronal mitochondria. This means CB1 receptors SLOW ECT transport and lower ATPase spin rate = lowered ATP content = mitochondria swell = loss of energy. These signals all favor apoptosis signaling in mitochondria. Since deuterium slows energy flux in mitochondria is appears the ECS and deuterium control mechanism are deeply linked in quantized fashion by sunlight. When the ECS system loses control of the ability to oxygenate PUFA’s all hell begins to break lose inside the matrix. This is why devastating hypoxia develops in ICU patients with C19.
Apoptosis normally destroys ECT in failing mitochondria. AM solar exposure increases both autophagy and apoptosis efficiency in mammalian cells. The release of the mitochondrial proteins and deuterium from failing mitochondrial membranes is the key sign of a failing powerhouse. It is a “quantum spin symptom” to the cell hierarchy that a brownout was under way so it was time to abort this mitochondria. Quantum spin problems are synonyms for the free radical pulses made in mitochondria.
HOW DOES SUNLIGHT THIN OUR BLOOD?
Solar exposure also improves the rheology of RBC and platelets to improve the laminar flow of blood and limit clotting. Both of these cells are without DNA because DNA is magnetic, so Nature made sure these two cell lines would not react to the magnetic effects of sunlight to harm us. Sunlight lowers blood pressure because it increases the free radical NO to dilate our arteriole beds. It is also a calcium channel blocker so it lowers blood pressure. Calcium dehydrates proteins and alters the aromatic amino acid mix in cells, to make neurohumoral chemicals that help optimize our physiology. Since sunlight exposure also thins out the blood, now you can understand why people with low Vitamin D 20(OH) tests have clotting disorders that seem to confound the conventional wisdom found of doctors in ICUs. Those patients have done worse with C-19 because of this lack of basic knowledge of why a lack of sun is among the greatest risk factors for C19 morbidity and mortality.
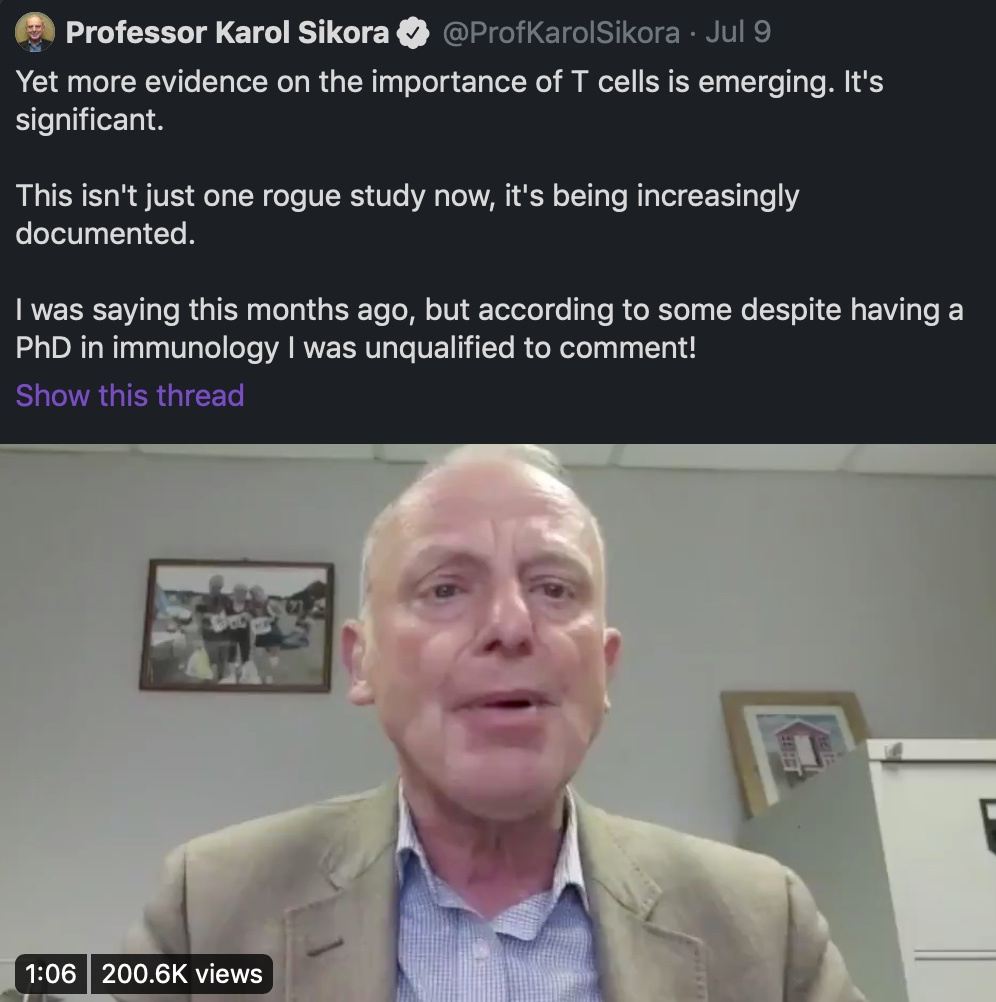
Most do not know that T cells are inherently magnetic because of the amount of ferritin they contain. This is why they become magnetized to pathogens EMF signals they react too. This locks them into their target pathogen and fever results and this leads to better killing of the invader. UV solar exposure unlocks their magnetic grip and allows the cells to limit the cytotoxic damage of the host. Note, most C19 deaths have been tied to cytotoxic storms being uncontrolled. Note that most deaths with C19 are linked to lowered Vitamin D levels. Note vitamin D is only made from UV light exposure.
Are you seeing a trend that a lack of UV light in your life might be a huge unrecognized problem?
Can T-cells work well on a planet with competing for magnetic field signals from tech gear?
Why are so many C-19 SARSCoV2 studies focusing on humoral immunity and neutralizing antibodies when B-cell antibody production is not crucial to overcome COVID19? It is the strong cytotoxic T-cell responses that bode well for long-term immunity. See when you ask the wrong questions you are destined to create the wrong answers for the unknowing public. This is what most people in public health have done with C-19. This is why they are advocating for a coronavirus vaccine. None of them tell you in human history there has never been ONE SUCCESSFUL human coronavirus vaccine.
Ask yourself why? Can they ever give you correct advice if they are looking at the wrong variables?
When clinical decisions become politicized, it’s politics as usual that gets amplified not the science buried in clinical medicine.
Again, de-magnetizing your blood via sunlight improves the fidelity of the Innate and Adaptive Cellular Immune systems. Moreover, this is the answer you should be seeking to C-19 and any other viral pathogens, known and unknown. How do we improve this arm of the immune system? Proper solar exposure = optimized T regulator cells function for the win!! Most of your T-cells are found in the skin in humans right where the sun hits it. This is why your skin needs to be in the game of Nature. Share this wisdom.
Consider joining my tribe at the URL KruseatDestin.com
I’m just warming up. It is summer and I am in the sun.