We do not produce anything worthwhile in medicine today. So it raises the interesting question, how does productivity measures relate to being a physician or a patient in 2018?? I do not think they relate to anything worthwhile in any circumstance. This meme was created by consultants from the business world that hospitals have used to usurp power from physicians. It is an apples to oranges comparison. Physicians work with individuals to diagnosis, prevent, treat, and hopefully improve both longevity and quality of life.
When doctors focus on productivity we begin to treat via our Rx pads and hospital algorithms/recipes built by the paradigm to harvest profits and not raise reversals of diseases. Moreover, in the process we’ve stopped educating our patients as we used to do. I changed that when I began blogging ten years ago. In my opinion, this is when we lose our edge our patients get more ill and their visits shorten because we have to trade time for money. Productivity of time leads to a paucity of good care.
According to Wikipedia, “Productivity describes various measures of the efficiency of production. A productivity measure is expressed as the ratio of output to inputs used in a production process, i.e., output per unit of input. Productivity is a crucial factor in production performance of firms and nations.”
Productivity is not a crucial factor to patients or doctors but it is to bean counters who are controlling hospitals and medical decisions in big government.
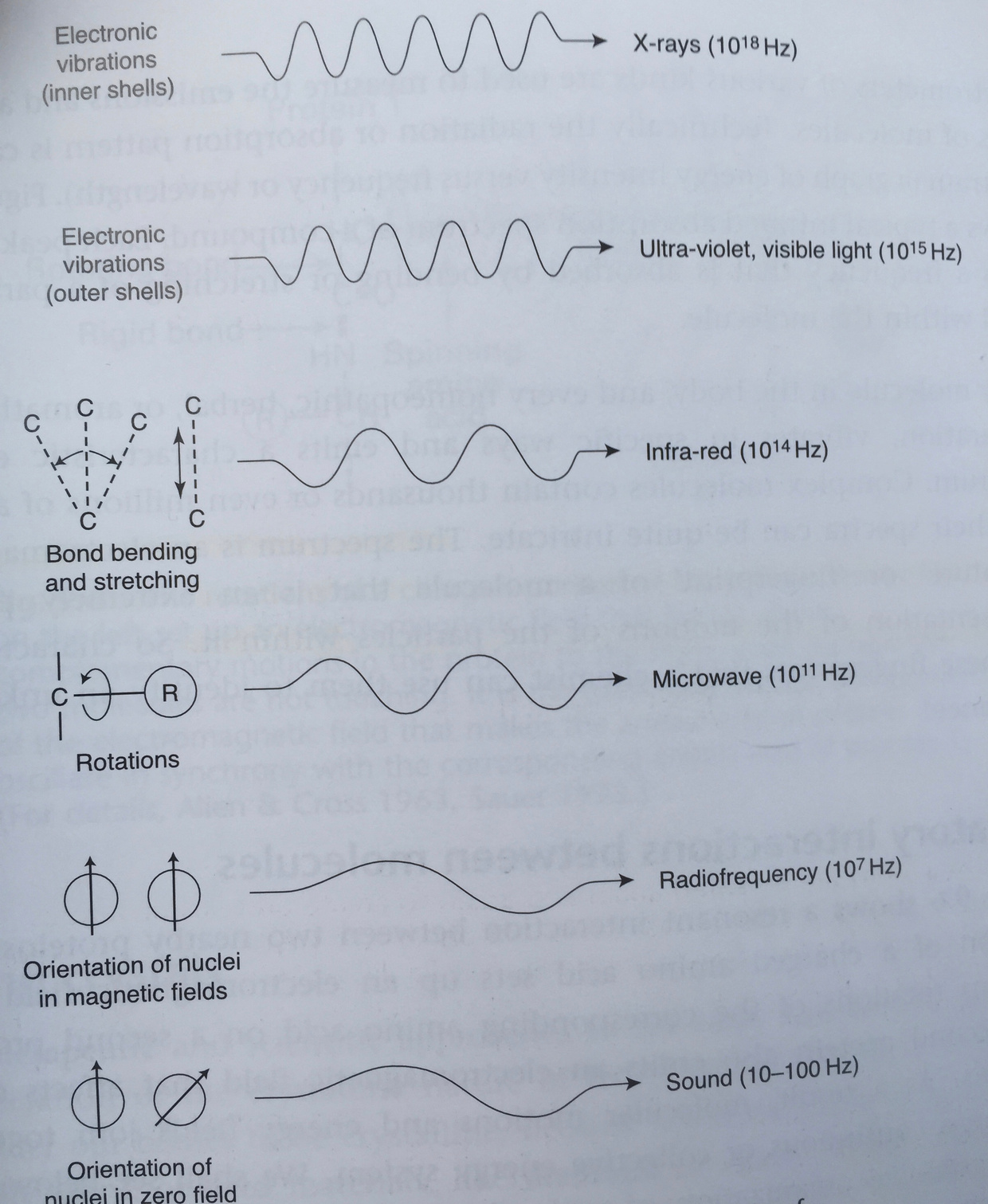
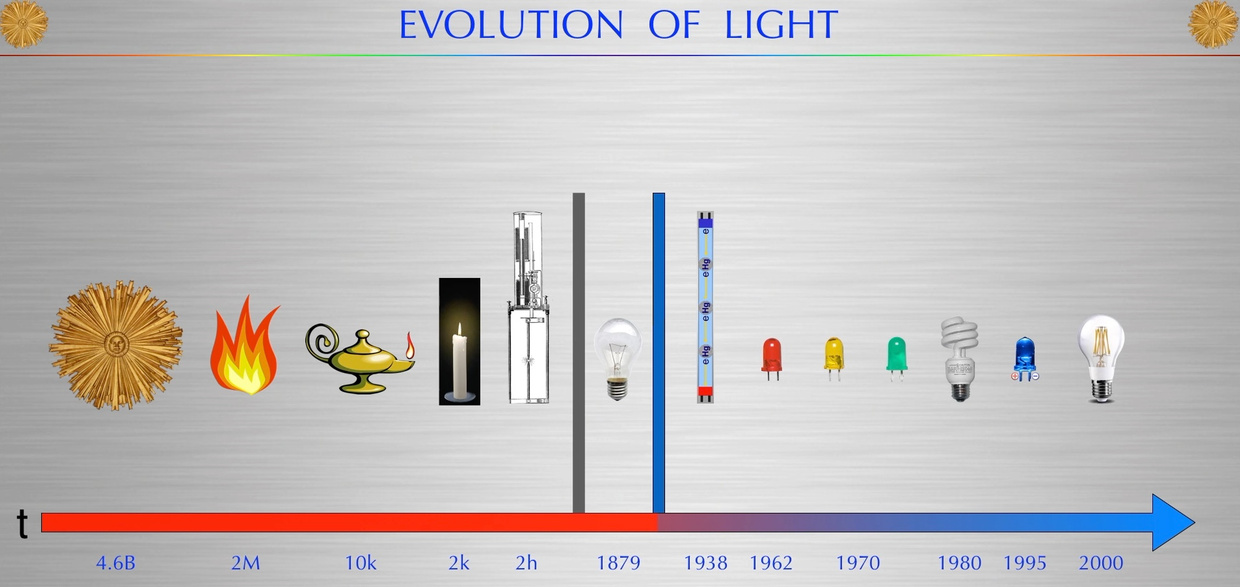
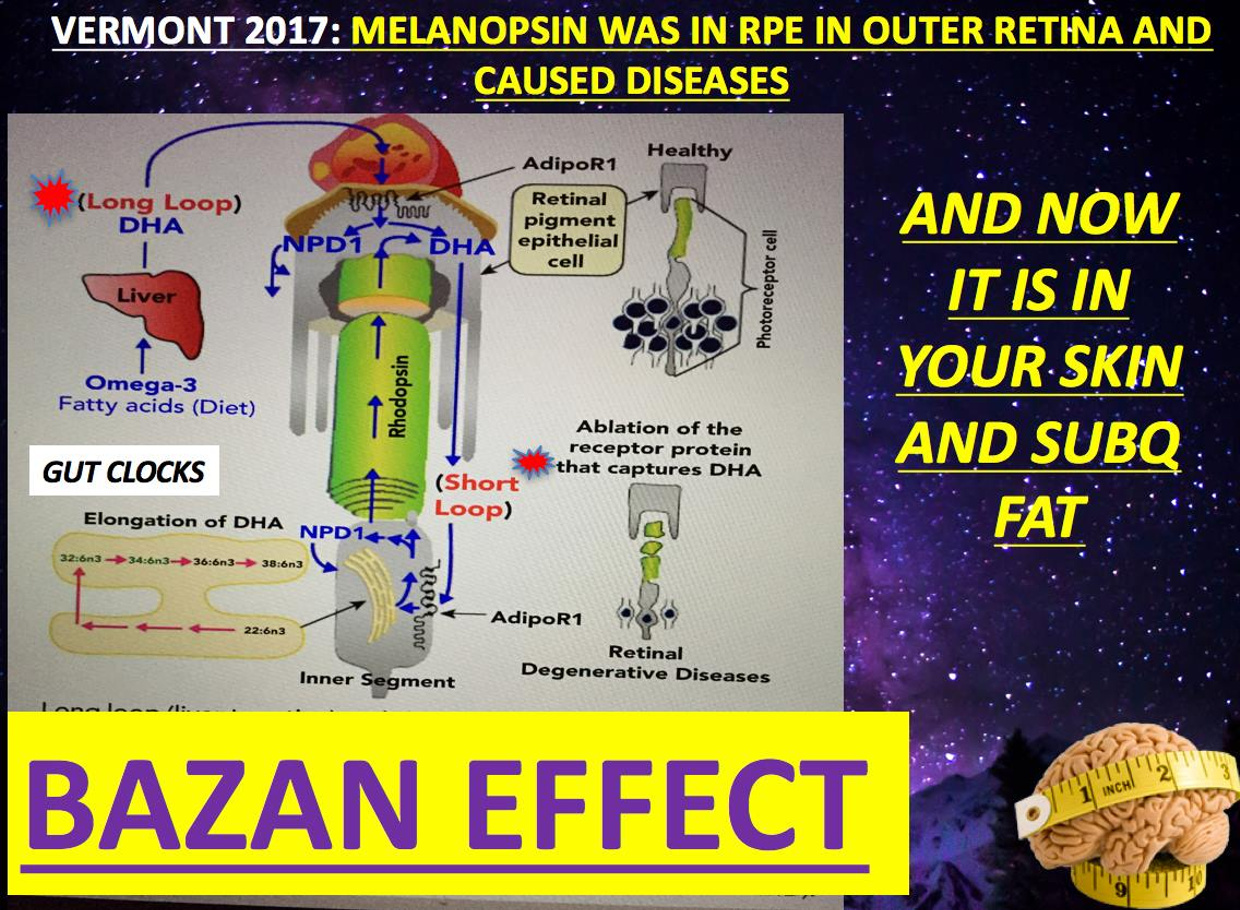
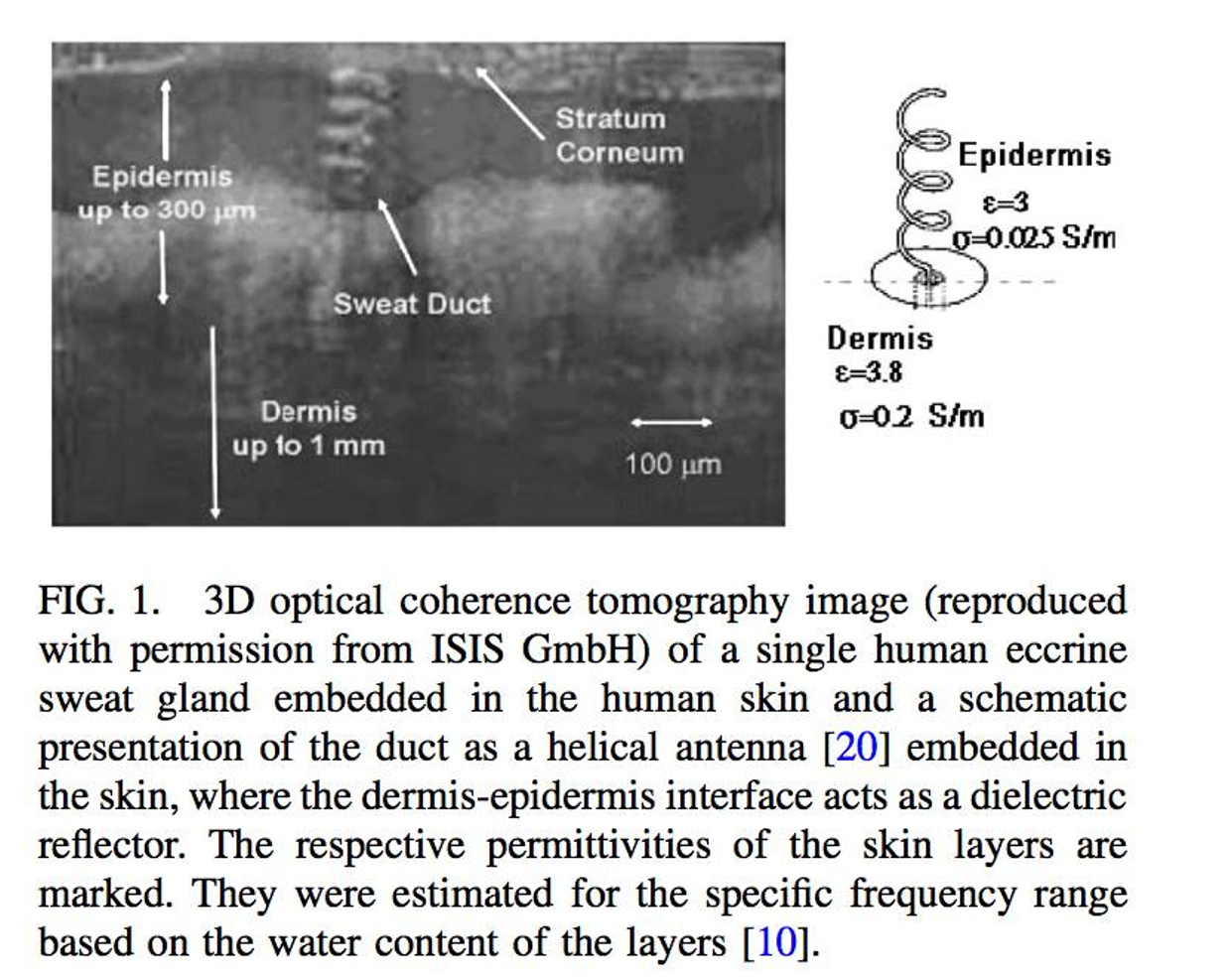
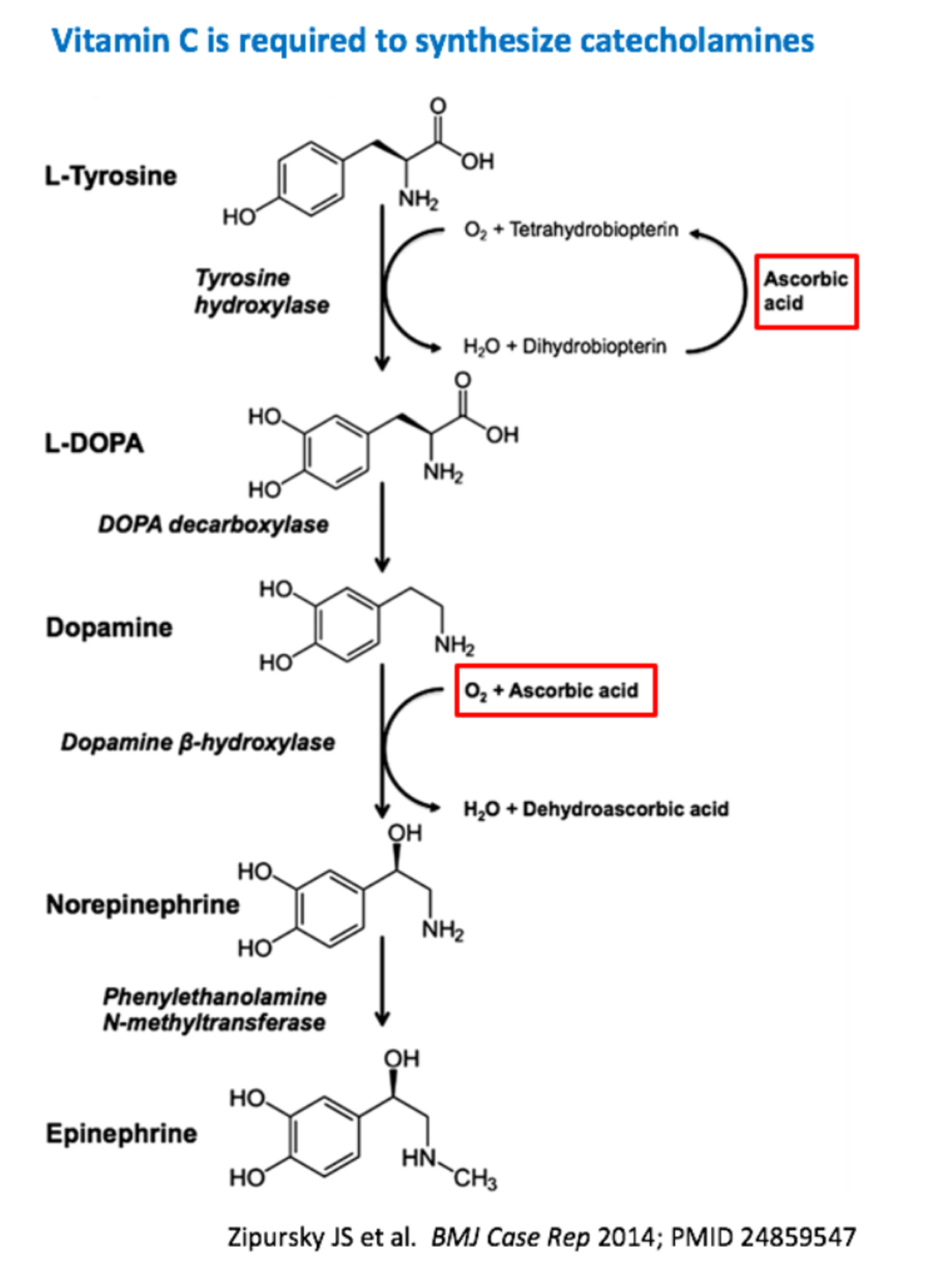
Hospitals build distractions in now for nurses, doctors, and patients via the electronic medical record. We now talk to screens and not to each other. This also increases the blue light hazard for all involved.
Being in a productive environment comes with its own challenges, such as the exposure of numerous distractions in the healthcare setting. Some of these include the constant influx of messages and emails from the EMR, which will then tempt you to answer them even if it isn’t necessary. Doing so can inhibit your productivity. In these cases, it’s necessary to make your environment conducive to productivity but this can’t always be the solution if your working environment is not in your own control. Today, we’ve lost control of the environment in medicine.
The players in healthcare also have lost much of their self discipline. Unfortunately, productivity doesn’t come naturally to some people because others are innately lacking in self-discipline. Without this trait, it will be challenging to create quality output in the space of time that makes it desirable. This is especially true in medicine. If a patient is not all in on their treatment plan, how good can we expect resutls to be. Conversely, if a doctor is treating people using the wrong ideas because evidence base algorithms’ are wrong how good will patients do in this paradigm? For example, a procrastinator MD may produce good results, but if the patient output can’t be produced within the required timeframe, because the patient has no skin in the game, it can seriously hamper productivity.
Physicians work with individual patients. We should strive to tailor care with our patients, and not some external stimulus. Sometimes that stimulus we bring to the table and it is completely counterproductive to the over success.
Productivity implies that we can count patient units. That idea really disrupts the essential “why” question?
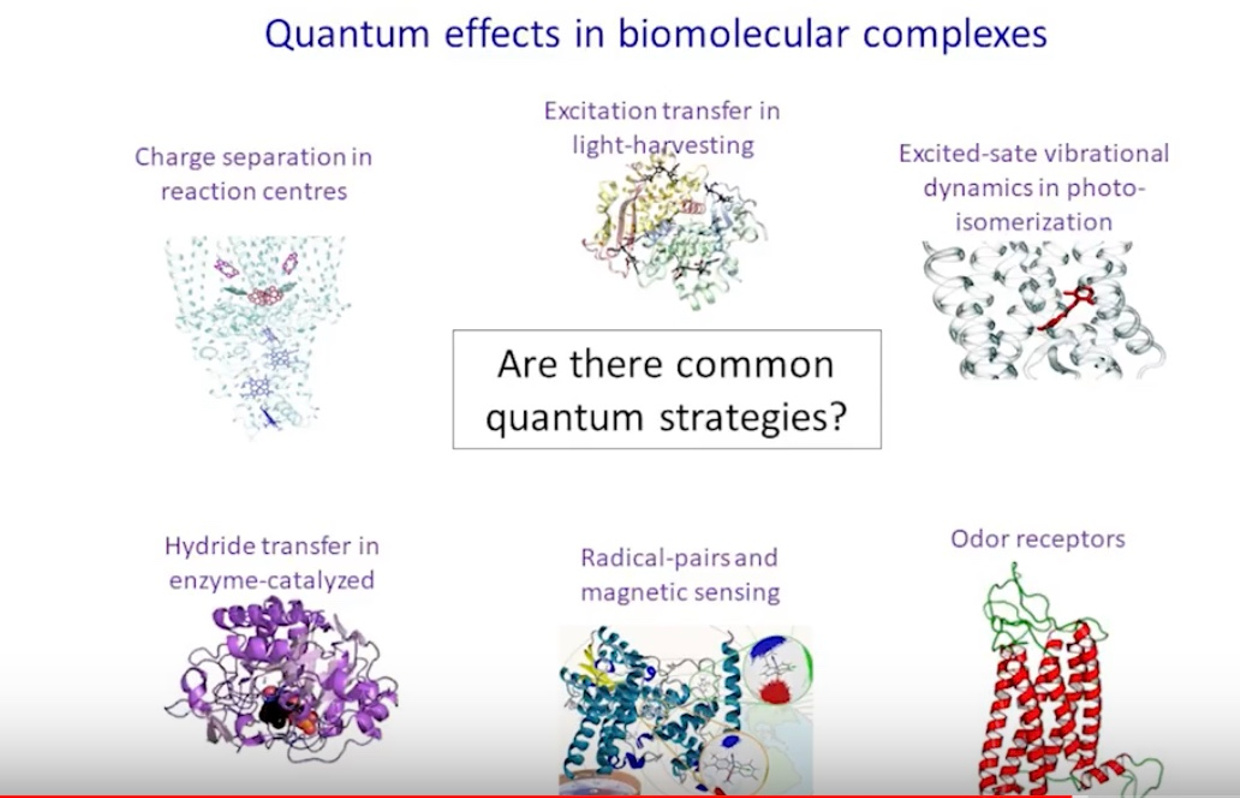
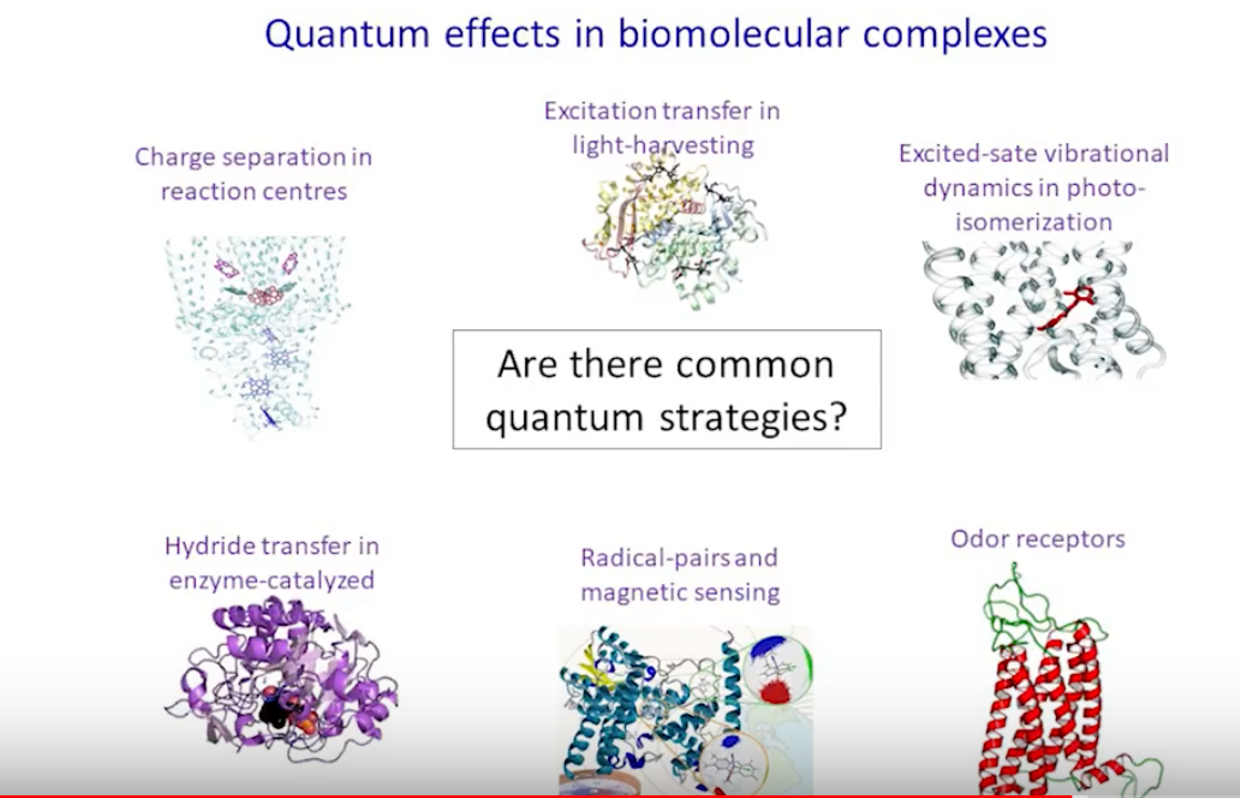
If you are unfamiliar with “why,” I highly recommend Simon Sinek’s book Start With Why. Why did we become physicians? Why have people become patients? Why did they choose us? I think about all these things now that I am a month away from opening up a Center that will focus on quantum biology. I think the answer for most physicians includes helping individual patients. We strive to do our best for each patient, but we need to reassess things and ask, are we really doing it? If not, why not?

Where did productivity measures enter medicine? It began when I was in medical school in the 1980’s. Most experts believe that Hsaio’s NEJM article, “Estimating Physicians’ Work for a Resource-Based Relative-Value Scale,” led to RVUs (relative value units) which many practice administrators use to measure “productivity.” Hsaio, a noted economist, wrote in the abstract of that article:
We found that physicians can rate the relative amount of work of the services within their specialty directly, taking into account all the dimensions of work. Moreover, these ratings are highly reproducible, consistent, and therefore probably valid.
This is where we really went off the rails in healthcare in my opinion. Why?
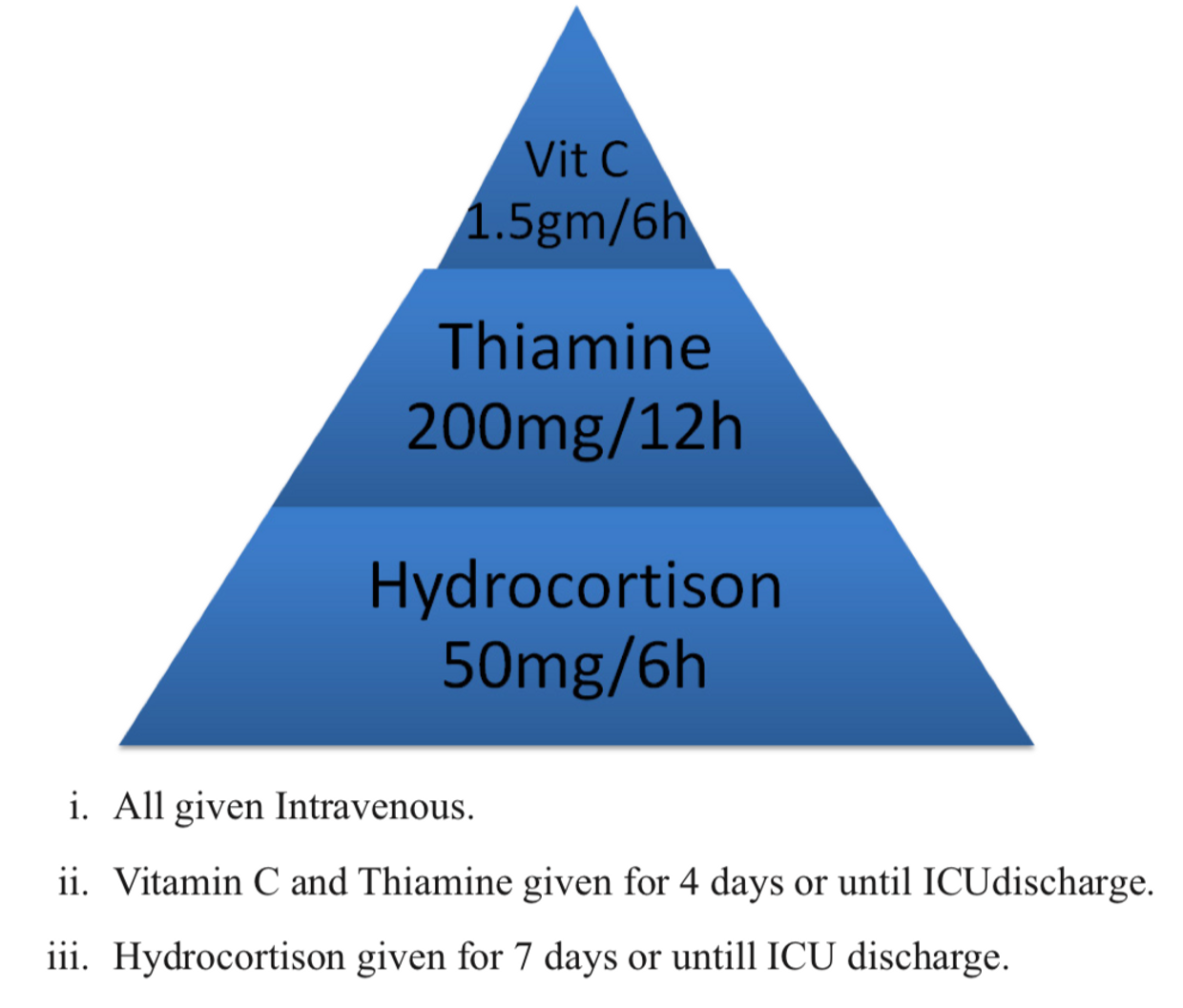
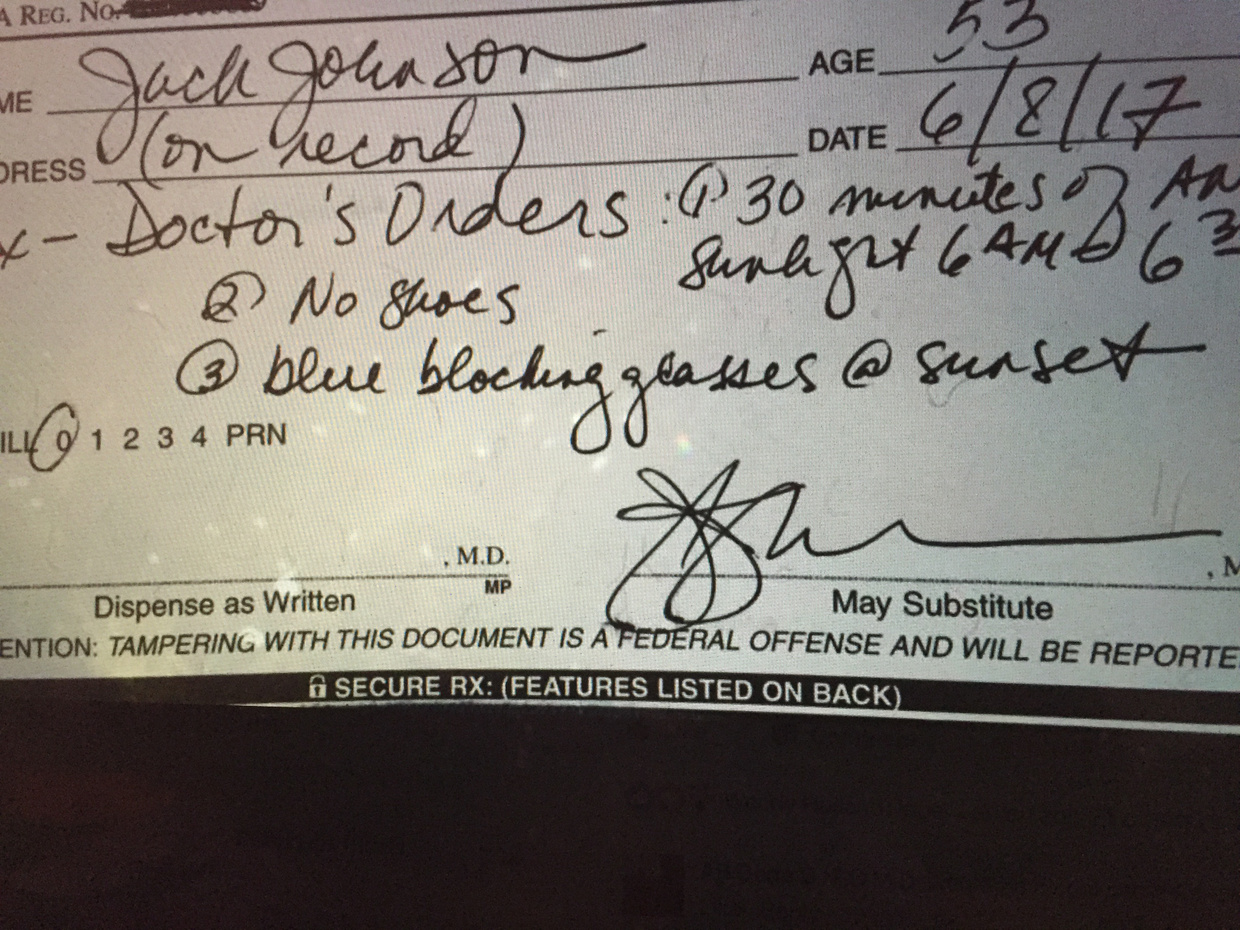
However, this model has led to gaming the system, and equating RVUs with hard work or productivity. But many physicians believe that the RVU system provides many wrong incentives, the most important being that shortening visit time leads to more patients per day and thus more money. I’d never get paid if I wrote this Rx for every patient because the paradigm has no rewards for prevention as a productivity measure, yet it is what patients all want.
I wish physicians could just ignore RVUs and spend appropriate time with each patient. When physicians try to do this, practice administrators work to get physicians to see patients faster.
This leads to great stress for many physicians, and often unhappy patients. Many physicians believe that shorter visits (especially with primary care physicians) lead to more testing and consultations. Functional medicine believes they solve the dilemma by expanding the visit but ordering massive amounts of tests they do nothing for outcome or productivity. They are making the same errors allopathic medicine has made by replacing testing and supplements for the prescription pad.
Productivity implies that seeing more patients each day is a good thing. But likely most patients and physicians will agree that we need to optimize the time with each patient. How many patients can we comfortably see in one day and deliver high-quality care? High-quality care does not refer to performance measures, but rather complex multi-dimensional factors that improve the patient experience. For many patients, talking about the things that really matter is both therapeutic and diagnostic. When we shorten our conversation time, and focus on the wrong things we raise the risk of diagnostic errors, while increasing health care costs, and create dissatisfied, confused patients. That is where we are now, because we’ve subtracted nature from medicine.
So please join my personal movement to ban technology productivity from medicine. Technology is ruining medicine for both doctors and patients We are not producing anything worthwhile in medicine right now. We need to be caring for patients who need our full attention in this world set up to harm them from technology and an indoor existence.